COVID-19 and Dietary Supplements: Evidence Tracker and Review 2021
Some doctors and media channels argue that there is very little evidence to support the use of dietary supplements to prevent or treat COVID-19. However, as of September 2021, there are more than 60 publications related to dietary supplements and COVID-19.
There are more than 80 types of supplements that are being studied for COVID-19. Vitamin D remains the most studied vitamin with the most evidence followed by zinc and vitamin C, for COVID-19. You can review the details of these trials on clinicaltrials.gov.
This guide is based on various references to scientific literature and hopefully, can help you make sense of the options and to separate the facts from fiction.
 |
| Image credit: ClevelandClinic |
Note: This is a highly dynamic topic; therefore, we will be updating this article as new information or evidence emerges.
Contents- Vitamin D3
- Quercetin
- Vitamin C
- Zinc
- Curcumin and Turmeric
- Melatonin
- NAC and Glutathione
- Omega 3 (Fish Oil)
- Selenium
- B Vitamins
- Molecular Hydrogen
- Lactoferrin
- Probiotics
- Green Tea (EGCG)
- Astaxanthin
- Vitamin D3
- Quercetin
- Vitamin C
- Zinc
- Curcumin and Turmeric
- Melatonin
- NAC and Glutathione
- Omega 3 (Fish Oil)
- Selenium
- B Vitamins
- Molecular Hydrogen
- Lactoferrin
- Probiotics
- Green Tea (EGCG)
- Astaxanthin
1. Vitamin D3
Vitamin D, whose forms are vitamin D2 and vitamin D3, is an essential nutrient that is naturally present in only a few foods, such as fatty fish (including salmon and tuna), fish liver oils, beef liver, cheese, and egg yolks. Fortified foods, especially fortified milk, provide most of the vitamin D in American diets. The RDA for vitamin D ranges from 10 to 15 mcg (400 international units [IU] to 600 IU) for children (depending on age) and from 15 to 20 mcg (600 to 800 IU) for adults. The body can also synthesize vitamin D from sun exposure.
Vitamin D obtained from sun exposure, foods, and supplements is biologically inert and must undergo two transformations in the body for activation. The first transformation, which occurs in the liver, converts vitamin D to 25-hydroxyvitamin D [25(OH)D]. The second transformation occurs primarily in the kidney and forms the physiologically active 1,25-dihydroxyvitamin D [1,25(OH)2D]. Serum concentration of 25(OH)D is currently the main indicator of vitamin D status. Although researchers have not definitively identified serum concentrations of 25(OH)D associated with deficiency and adequacy, the FNB advises that levels below 30 nmol/L (12 ng/mL) are associated with vitamin D deficiency, and levels of 50 nmol/L (20 ng/mL) or more are considered adequate for bone and overall health in most people [Source].
In addition to its well-known effects on calcium absorption and bone health, vitamin D plays a role in immunity [Source]. Vitamin D appears to lower viral replication rates, suppress inflammation, and increase levels of T-regulatory cells and their activity. In addition, immune cells (e.g., B lymphocytes and T lymphocytes) express the vitamin D receptor and some immune cells (e.g., macrophages and dendritic cells) can convert 25(OH)D into the active 1,25(OH)2D. This ability suggests that vitamin D might modulate immune responses.
Vitamin D and COVID-19
Based on several publications and studies, vitamin D seems to be the “most promising” natural supplement for COVID-19 protection. Vitamin D deficiency is known to enhance a process known as the “cytokine storm” (Marik, Jun 2020).
In a study (Frontiers in Immunology, Dec 2020) using bioinformatics and systems biology approach, the pathways associated with cytokine storm in COVID-19 is identified and suggested that the underlying mechanism of vitamin D could be promising in suppressing the cytokine storm.
A meta-analysis of 43 vitamin D observational studies (Petrelli, March 2021) points to effectiveness against COVID-19. Two studies in France (C Annweiler, Nov 2020; G Annweiler, Nov 2020), one in India (A Rastogi, Nov 2020) and one in Spain (M Castillo, Oct 2020) showed that Vitamin D supplementation seems to decrease the mortality rate, the severity of the disease, and the inflammatory markers' levels among the COVID-19 infected patients, leading to a better prognosis and increased survival.
In a study from Nature (Sci Rep, May 2021) to investigate the effects of daily high-dose supplementation (60,000 IUs) of vitamin D — for eight to 10 days, in addition to standard therapy, for COVID-19 patients deficient in vitamin D; Vitamin D levels increased significantly in the vitamin D group — from 16 ng/ml to 89 ng/ml — while inflammatory markers significantly decreased, without any side effects.
The largest observational study to date, looked at data for 191,779 American patients who were tested for SARS-CoV-2 between March and June 2020 and had had their vitamin D tested sometime in the preceding 12 months.
Of those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested positive for SARS-CoV-2, compared to 8.1% of those who had a vitamin D level between 30 and 34 ng/ml (adequacy) and 5.9% of those who had an optimal vitamin D level of 55 ng/ml or higher.
Of those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested positive for SARS-CoV-2, compared to 8.1% of those who had a vitamin D level between 30 and 34 ng/ml (adequacy) and 5.9% of those who had an optimal vitamin D level of 55 ng/ml or higher.
A study published in November 2020 from Singapore (CW Tan, Nutrition 2020), found that those who were started on a daily oral dose of vitamin D3 (1,000 IU), magnesium (150 mg) and vitamin B12 (500 mcg) within the first day of hospitalisation and continued up to 14 days were significantly less likely to require oxygen therapy and further intensive care.
According to the statement released on 2 October 2020 by the U.S. president’s physician said that in addition to the antibodies, Trump “has been taking zinc, vitamin D, famotidine, melatonin and a daily aspirin.”
Another study, published in JAMA (JAMA Netw Open - Sep 2020) found that persons who are likely to have deficient vitamin D levels at the time of COVID-19 testing were at substantially higher risk of testing positive for COVID-19 than were persons who were likely to have sufficient levels.
There are many vitamin D studies underway. You can review the status of these trials on clinicaltrials.gov. As of July 2021, more than 40 studies have been launched to investigate the benefits of vitamin D against COVID-19.
Another study, published in JAMA (JAMA Netw Open - Sep 2020) found that persons who are likely to have deficient vitamin D levels at the time of COVID-19 testing were at substantially higher risk of testing positive for COVID-19 than were persons who were likely to have sufficient levels.
A study of 20 European countries found a link between low levels of vitamin D and higher percentages of COVID-19 cases and mortality. Separately, more than 80% of 200 people hospitalized for COVID-19 in Spain were found to be deficient in vitamin D, according to a study published in October 2020 in the Journal of Clinical Endocrinology & Metabolism.
A review by Dinicolantonio et al (Mo Med Feb 2021) also suggested vitamin D and magnesium deficiency as a potential cause of cytokine storm in COVID-19 patients and recommended that vitamin D and magnesium supplementation to be considered.
Check out the evidence tracker on vitamin D and COVID-19 from c19vitamind.com (constantly updated).
2. Quercetin
Quercetin is a pigment that is found in plants, vegetables, and fruits, and serves as an immune nutrient offering many health benefits. Elderberry, red onions, white onions and cranberries are the richest sources of quercetin. It is a flavonoid and antioxidant that may help to reduce inflammatory cytokines, infections, allergies and anti-blood clot property. Research has found that quercetin may be particularly beneficial for viral respiratory infections.Quercetin and COVID-19
An Italo-Pakistani, randomized trial of Quercetin (Di Pierro et al 2021) in high bioavailability form in Covid outpatients (n=152) yields spectacular results that beg for immediate reproduction: > 68% less hospitalizations, which are 78% shorter and 100% less ICU admissions or deaths.
There is evidence that vitamin C and quercetin co-administration exerts a synergistic antiviral action due to overlapping antiviral and immunomodulatory properties and the capacity of ascorbate to recycle quercetin, increasing its efficacy.
As of September 2021, more than 10 studies have been launched to investigate the benefits of quercetin against COVID-19. Ultimately, the results of the above trials will offer more definitive evidence.
Quercetin was initially found to provide broad-spectrum protection against SARS coronavirus in the aftermath of the SARS epidemic that broke out across 26 countries in 2003. Now, some doctors are advocating its use against SARS-CoV-2, in combination with vitamin C, noting that the two have synergistic effects.
Quercetin, Vitamin C, D, Zinc and Melatonin - FLCCC I-MASK+ Protocol
Incidentally, ascorbic acid (vitamin C) and the bioflavonoid quercetin (originally labeled vitamin P) were both discovered by the same scientist — Nobel prize winner Albert Szent-Györgyi. Quercetin and vitamin C also act as an antiviral drug, effectively inactivating viruses.
There is evidence that vitamin C and quercetin co-administration exerts a synergistic antiviral action due to overlapping antiviral and immunomodulatory properties and the capacity of ascorbate to recycle quercetin, increasing its efficacy.
For updated prevention and early outpatient protocol for COVID-19 positive, please check out FLCCC I-MASK+ protocol.
Related: Best Pulse Oximeter 2021
Quercetin, Zinc, Vitamin D and C: AAPS (Association of American Physicians and Surgeons) Guidelines
The AAPS recommends the following outpatient nutraceutical 'treatment' protocol for COVID-19:
Please take note the above dosages are relatively high and is meant for 'treatment'. If you wish to continue taking these nutrients for health maintenance, you'll need to reduce the dosages based on the recommended dietary allowance (RDA or RDI) after you've recovered.
A word about quercetin: Some physicians are recommending this supplement to reduce viral illnesses because quercetin acts as a zinc ionophore to improve zinc uptake into cells. It is much less potent than HCQ (hydroxychloroquine) as a zinc transporter, and it does not reach high concentrations in lung cells that HCQ does. Quercetin may help reduce risk of viral illness if you are basically healthy. But it is not potent enough to replace HCQ for treatment of COVID once you have symptoms, and it does not adequately get into lung tissue unless you take massive doses (3-5 grams a day), which cause significant GI (gastrointestinal) side effects such as diarrhea.
Related: Best Quercetin Zinc Supplement
3. Vitamin C
Vitamin C may be one of the most well-known immune nutrients that protect against immune deficiencies and which supports the prevention and recovery from the common cold and upper-respiratory issues, and also protects your cardiovascular system, eyes, skin, and other parts of your body. Research has found that vitamin C may help to optimize the immune system.Vitamin C and COVID-19
Most people turn to vitamin C after they've caught a cold. That’s because it helps build up your immune system. Vitamin C is thought to increase the production of white blood cells. These are key to fighting infections. Some of the most vitamin C-rich foods include citrus fruits, from tangerines to limes, along with leafy greens, bell peppers, papaya and broccoli. Berries are another great source, and they all provide this and other potent antioxidants, which support your immune response and help to rebuild collagen. Because your body doesn't produce or store it, you need daily vitamin C for continued health. Almost all citrus fruits are high in vitamin C.
Safety: Taking large doses of vitamin C (ascorbic acid) on a regular basis lowers your level of copper, so if you are already deficient in copper and take high doses of vitamin C, you can compromise your immune system.
Temporarily taking megadoses of vitamin C supplements to combat a case of the cold or flu is likely not going to cause a problem.
Many vitamin C supplements that are above the US RDA are sold in the market. It’s important to seek a physician’s advice if you intend to take high dose vitamin C on a long term basis. To be on the safe side, you may also request for your kidney functions to be monitored.
For long-term, daily use, your best bet is to eat a diet that is full of high quality organic vegetables and fruits that are minimally processed. Not only will you get vitamin C, but you will get all the other accessory nutrients and micronutrients that are needed to optimize it.
There are many vitamin C studies underway and you can review the status of these trials on clinicaltrials.gov. As of July 2021, there are more than 20 studies that have been launched to investigate the benefits of vitamin C against COVID-19.
Vitamin C might help prevent COVID-19 and also lessen the inflammatory reactions behind some severe COVID-19 cases, according to a review of research on the topic published in the latest issue of the journal Nutrition.
Check out the evidence tracker on vitamin C and COVID-19 from c19vitaminc.com (constantly updated).
The U.S. Recommended Dietary Allowance (RDA) for vitamin C is 75 to 120 milligrams per day.
Safety: Taking large doses of vitamin C (ascorbic acid) on a regular basis lowers your level of copper, so if you are already deficient in copper and take high doses of vitamin C, you can compromise your immune system.
While generally considered safe even in high doses, way too much vitamin C — anything above 2,000 milligrams daily—can cause headaches, insomnia, diarrhea, heartburn, and other issues.
Temporarily taking megadoses of vitamin C supplements to combat a case of the cold or flu is likely not going to cause a problem.
Related: Best Vitamin C Supplements 2021
4. Zinc
Zinc is another powerful immune nutrient known for its benefits for providing immune health support and inflammation reduction as well as for improving cold and respiratory symptoms, wound healing, acne reduction, and lowering the risk of age-related diseases. Research on atherosclerosis and diabetes mellitus suggests that zinc deficiency may contribute to low-grade systemic inflammation.
Aging is associated with compromised immunity, that just means that your immune response to pathogens and infections starts to slow and is less robust, including a reduced vaccine immune response/efficacy.
Improving zinc intake/zinc status improves/modulates/enhances immune function. The flip side is, while some aspects of immunity slow, others increase. Uncontrolled immune responses drive excess inflammation. Zinc helps to balance all of this.
Improving zinc intake/zinc status improves/modulates/enhances immune function. The flip side is, while some aspects of immunity slow, others increase. Uncontrolled immune responses drive excess inflammation. Zinc helps to balance all of this.
Zinc and COVID-19
Interestingly, some researchers have proposed low zinc status may contribute to the loss of smell that sometimes accompanies respiratory viral infections (J Clin Biochem Nutr. 2021 Jan); while one study found no significant relationship between zinc status and loss of smell in 134 patients with a viral respiratory infection, it did note those who received 50 mg elemental zinc twice daily recovered their sense of smell more quickly than those who received no zinc (Abdelmaksoud et al. 2021 Jan).
There are many Zinc studies underway and you can review the status of these trials on clinicaltrials.gov. As of April 2021, there are more than 20 studies that have been launched to investigate the benefits of Zinc against COVID-19.
Zinc has been shown in a lab study to inhibit regular coronavirus (not the current SARS-CoV-2) since 2010, in a 2010 publication.
Check out the evidence tracker on zinc and COVID-19 from c19zinc.com (constantly updated).
Safety: Taking zinc long term is typically safe for healthy adults, as long as the daily dose is under the set upper limit of 40 mg of elemental zinc (PubMed). Be aware that typical daily doses of zinc provided by zinc lozenges generally exceed tolerable upper limits for zinc, and for this reason, they should not be used for longer than about a week.
Excessive doses may interfere with copper absorption, which could negatively affect your immune system as it can cause copper deficiencies, blood disorders and potentially permanent nerve damage. Zinc can also impair the absorption of antibiotics, and use of zinc nasal gels or swabs has been linked to temporary or permanent loss of smell.
The ideal dose for prevention while the COVID-19 risk is high is 40-100 mg/d, a portion of which comes from zinc lozenges to spread the zinc through the tissues of the nose, mouth and throat. It should be accompanied by at least 1 mg copper from food and supplements for every 15 mg zinc.
Do take note that you should keep the dosage back to within 40 mg/d once the exposure risk is back to normal.
5. Curcumin and Turmeric
Curcumin, a yellow carotenoid from turmeric, is well known for its anti-inflammatory and free radical-scavenging effects.Curcumin and COVID-19
It has also demonstrated antiviral effects against a range of respiratory viruses, including influenza A virus and others (Ref). Computer models suggest curcumin may interfere with viral entry into cells as well as viral replication inside cells (Ref). Numerous preclinical studies indicate curcumin may activate antiviral immunity; at the same time, curcumin appears to inhibit infection-induced inflammatory signaling and promote anti-inflammatory processes, reducing the potential for a cytokine storm and ARDS and protecting other organ systems (Ref). By suppressing inflammation, curcumin has the potential to help mitigate complications and sequelae of severe acute viral respiratory infections (Ref).
Curcumin has been demonstrated (Ref) to suppress several inflammatory cytokines and mediators of their release such as tumor necrosis factor-alpha (TNF-alpha), IL-1, IL-8 and nitric oxide synthase.
In an open-label trial, 21 patients hospitalized with mild-to-moderate illness due to a highly infectious respiratory virus were treated with a nano-curcumin preparation providing 80 mg curcuminoids (curcumin and its related compounds) twice daily for two weeks in conjunction with standard therapies; their progress was compared with 20 similar patients treated with standard therapies alone. Those who received curcumin had better oxygenation status beginning on day two of treatment, as well as faster resolution of most symptoms, faster normalization of immune cell numbers, less likelihood of worsening of their clinical status, shorter time requiring supplemental oxygen, and shorter hospital stays (Ref).
In a double-blind placebo-controlled trial of 40 participants with a viral respiratory illness, those who received 160 mg nano-curcumin per day for 14 days along with standard therapy had greater reductions in some inflammatory cytokines, including IL-6. They also experienced significant improvement in more symptoms and had a lower fatality rate than those receiving placebo (Ref).
In an open-label trial, 21 patients hospitalized with mild-to-moderate illness due to a highly infectious respiratory virus were treated with a nano-curcumin preparation providing 80 mg curcuminoids (curcumin and its related compounds) twice daily for two weeks in conjunction with standard therapies; their progress was compared with 20 similar patients treated with standard therapies alone. Those who received curcumin had better oxygenation status beginning on day two of treatment, as well as faster resolution of most symptoms, faster normalization of immune cell numbers, less likelihood of worsening of their clinical status, shorter time requiring supplemental oxygen, and shorter hospital stays (Ref).
In a double-blind placebo-controlled trial of 40 participants with a viral respiratory illness, those who received 160 mg nano-curcumin per day for 14 days along with standard therapy had greater reductions in some inflammatory cytokines, including IL-6. They also experienced significant improvement in more symptoms and had a lower fatality rate than those receiving placebo (Ref).
The same research group conducted another double-blind placebo-controlled trial in hospitalized patients with the same virulent respiratory virus, 40 with severe illness receiving intensive care and 40 with mild illness; half of the participants in each group received 160 mg nano-curcumin per day for 14 days and the other half received placebo. Curcumin-treated patients had lower numbers and activity of immune cells known to be involved in cytokine storm and hyper-inflammation. They also had greater improvement in fever, cough, and shortness of breath, and had lower mortality rates (0% vs. 5% in those with mild illness and 5% vs. 25% in those with severe illness [p<.0001 for both mild and severe cases]) than those who received placebo (Ref).
6. Melatonin
Melatonin is a hormone produced by the pineal gland in the brain, mainly during the night, that helps regulate circadian rhythms [Source]. Its levels decrease with aging. Most melatonin supplementation studies have evaluated its ability to control sleep and wake cycles, promote sleep, and reduce jet lag.
Laboratory and animal studies suggest that melatonin enhances immune response by increasing the proliferation and maturation of natural killer cells, T and B lymphocytes, granulocytes and monocytes . Melatonin also appears to have anti-inflammatory and antioxidant effects [Source]. However, whether these properties have a clinically significant effect on immunity in humans is not clear.
Laboratory and animal studies suggest that melatonin enhances immune response by increasing the proliferation and maturation of natural killer cells, T and B lymphocytes, granulocytes and monocytes . Melatonin also appears to have anti-inflammatory and antioxidant effects [Source]. However, whether these properties have a clinically significant effect on immunity in humans is not clear.
Melatonin and COVID-19
The potential utility of melatonin in treating COVID patients has not gone unnoticed, with a PubMed search combining melatonin and COVID producing more than 50 citations.
Assisting sleep and rest is already an immune system-supporting benefit, but melatonin has more to offer. It is a powerful antioxidant that supports your immune health, brain, eyes, digestion, and more. It may even be helpful when it comes to COVID-19.
As discussed in a review (Cardinali et al. 2020), melatonin might counteract the consequences of COVID-19 via salutary effects on the sleep/wake cycle and more generally on chronobiology, as well as through its antioxidant and anti-inflammatory effects.
Based on melatonin’s therapeutic potential and well-established safety profile, it has been suggested those at higher risk for severe illness and complications from viral respiratory infection, including the elderly and those with chronic medical conditions, may benefit most from regular use of 3–10 mg melatonin at bedtime (Ref).
Fluvoxamine (Selective Serotonin Reuptake Inhibitor) might also exert beneficial effects in COVID patients through its well-characterized ability to substantially increase (~ 2–3-fold) night-time plasma levels of melatonin. This increase appears to result from fluvoxamine’s inhibition of the melatonin-metabolizing liver enzymes (von Bahr et al. 2000).
An Iranian randomised controlled trial (Arch Med Res 2021), studied 74 mild to moderate hospitalized patients. The study showed that adjuvant use of melatonin has a potential to improve clinical symptoms of COVID-19 patients and contribute to a faster return of patients to baseline health.
"Patients who used melatonin as a supplement had, on average, a 28% lower risk of testing positive for SARS-CoV-2. Blacks who used melatonin were 52% less likely to test positive for the virus."
Some researchers have suggested high doses of melatonin, ranging from 50 to 200 mg twice daily, might help treat patients hospitalized for severe acute respiratory illness (Ref).
In a small Philippine case series study of 10 hospitalised COVID-19 patients, high dose melatonin (hdM) was given in addition (adjuvant) to standard therapy. According to the authors:
"High dose melatonin may have a beneficial role in patients treated for COVID19 pneumonia, in terms of shorter time to clinical improvement, less need for MV, shorter hospital stay, and possibly lower mortality."
Melatonin supplementation may reduce the risk of acute viral respiratory infections, help mitigate some chronic health problems that increase infection vulnerability, and protect against neurological and cardiovascular complications of viral respiratory infections (Reiter et al. 2020).
In another observational study that followed 11,672 individuals, melatonin use was associated with a reduced risk of testing positive for a common, highly infectious respiratory virus (Ref).
Another study looked at data from 791 patients intubated for respiratory support during an outbreak of a severe acute viral respiratory illness and 2,981 patients needing the same level of respiratory support for other reasons. The use of melatonin, most often for sleep issues, during the intubation period was associated with significantly improved outcomes in both groups and increased the likelihood of survival in virus-infected patients who required mechanical ventilation (Ref).
As of July 2021, more than 8 studies are currently underway to investigate the benefits of melatonin against COVID-19. Ultimately, the results of the above trials will offer more definitive evidence.
Typical doses of 1–10 mg/day melatonin appear to be safe for short-term use (Source). Reported side effects, which are usually minor, include dizziness, headache, nausea, upset stomach, rash, and sleepiness. However, some reports have linked high blood levels of melatonin with delayed puberty and hypogonadism.
Studies have not evaluated melatonin supplementation during pregnancy and breastfeeding, but some research suggests that these supplements might inhibit ovarian function (Source). Therefore, some experts recommend that women who are pregnant or breastfeeding avoid taking melatonin.
Much of the research on NAC has used an inhaled, liquid form of this compound. This form—which is classified as a drug, not a dietary supplement—is approved by the U.S. Food and Drug Administration (FDA) as a mucolytic agent and for decreasing respiratory secretion viscosity (Source). Products containing NAC are also sold as dietary supplements.
Safety: As an FDA-approved drug, the safety profile of NAC has been evaluated (Source) [88]. Reported side effects of oral NAC include nausea, vomiting, abdominal pain, diarrhea, indigestion, and epigastric discomfort (Source). No safety concerns have been reported for products labeled as dietary supplements that contain NAC.
3. Vitamin D3 5000iu 1 time a day for 7 days (Amazon)
Omega-3s play important roles as components of the phospholipids that form the structures of cell membranes (Source). Omega-3s also form eicosanoids; these signaling molecules affect the body’s cardiovascular, pulmonary, immune, and endocrine systems. Omega-6 fatty acids, the other major class of polyunsaturated fatty acids, also form eicosanoids, and these eicosanoids are generally more potent mediators of inflammation, vasoconstriction, and platelet aggregation than those made from omega-3s. Thus, higher concentrations of omega-3s than of omega-6s tip the eicosanoid balance toward less inflammatory activity.
Higher intakes and blood levels of EPA and DHA are associated with lower levels of inflammatory cytokines (Source). Omega-3s might also affect immune function by up-regulating the activity of macrophages, neutrophils, T cells, B cells, natural killer cells, and other immune cells.
"Among these micronutrients, LC-PUFAs (long-chain polyunsaturated fatty acids) such as EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are noteworthy because of their direct influence in the immunological response to viral infections.
Among these complex immunomodulatory effects, interleukin-6 (IL-6) and interleukin-1ß (IL-1β)—because of the suspected central regulatory role in the "cytokine storm"—should be highlighted."
The omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) modulate inflammatory processes in the body through a variety of mechanisms (Ref, Ref). Severe acute viral respiratory infections can sometimes trigger cytokine storm, in which excessive production of inflammatory cytokines leads to uncontrolled systemic inflammation and life-threatening tissue and organ damage. Another phenomenon, called eicosanoid storm, has also been proposed to contribute to widespread inflammation, tissue damage, and organ failure. Eicosanoid storm is characterized by excessive production of pro-inflammatory and procoagulant eicosanoids made from arachidonic acid, an omega-6 fatty acid synthesized in the body and obtained from dietary animal fat (Ref, Ref). By competing with arachidonic acid for metabolic enzymes, EPA and DHA decrease the production of pro-inflammatory and procoagulant eicosanoids and increase production of specialized inflammation-resolving compounds (Ref, Ref).
Accumulating evidence shows omega-3 fatty acids, administered orally or intravenously, may help control inflammation and improve outcomes in critically ill patients, including those with ARDS.489 A meta-analysis of 12 randomized controlled trials with a total of 1,280 critically ill patients with ARDS found supplementation with omega-3 fatty acids, in combination with gamma-linolenic acid (a less-inflammatory omega-6 fatty acid) and antioxidants, improved markers of lung function; however, only hourly administration, rather than large bolus intravenous dosing, was associated with reduced mortality. Although reductions in mechanical ventilation and length of stay in intensive care were seen, these effects did not reach statistical significance (Ref).
An observational study in 100 patients hospitalized with a severe acute viral respiratory illness found higher levels of EPA plus DHA were associated with lower mortality, though the effect was not statistically significant, possibly due to the small number of participants (Ref). During an outbreak of a severe viral respiratory infection, another study found countries with the highest intake of omega-3 fatty acids from marine sources had lower mortality rates than other regions of the world (Ref). The same research group used computer modeling to show how omega-3 fatty acids might bind to the highly infectious virus and interfere with its ability to enter cells (Ref).
Self-reported use of omega-3 supplements (dose not reported) more than three times per week for at least 3 months among 372,720 U.K. residents aged 16 to 90 years was associated with a 12% lower risk of SARS-CoV-2 infection after adjustment for potential confounders (Source). Findings were similar for 45,757 individuals in the United States and for 27,373 participants in Sweden.
That are more than a dozen studies on-going that examine the effect of EPA and/or DHA on the prevention of or lessening of symptoms of COVID-19.
EPA and DHA have a direct influence in the immunological response to viral infections and can modulate immune response and function.
Animal-based omega-3 fats, especially DHA, also help prevent thrombosis (a blood clot within a blood vessel) by decreasing platelet aggregation. Hypercoagulation is another complication of severe COVID-19 infection that can have lethal consequences.
Omega-3 also lowers your risk of lung dysfunction, protects against lung damage and secondary bacterial infections, and improves mitochondrial function.
Research shows that by lowering triglycerides, the risk of developing a cytokine storm is diminished. Omega-3 supplementation is known to lower triglycerides, but krill oil does so more effectively than fish oil.
An interesting development published in Science, Nov 2020 revealed that linoleic acid (omega-6) binds with the 'spike protein' of the COVID-19 virus and interferes with the entrance of the virus into a human cell via the ACE-2 receptors. The study also revealed that in human cells, Linoleic Acid supplementation synergizes with the COVID-19 drug remdesivir in suppressing SARS-CoV-2 replication.
Safety: The FDA recommends not exceeding 3 g/day EPA and DHA combined, including up to 2 g/day from dietary supplements (Source). Some doses used in clinical trials exceed these amounts. The FNB did not establish a Tolerable Upper Intake Level (UL; maximum daily intake unlikely to cause adverse health effects) for omega-3s, although it noted that high doses of DHA and/or EPA (900 mg/day EPA plus 600 mg/day DHA or more for several weeks) might reduce immune function by suppressing inflammatory responses (Source).
Commonly reported side effects of omega-3 supplements—including unpleasant taste, bad breath, heartburn, nausea, gastrointestinal discomfort, diarrhea, headache, and odoriferous sweat—are usually mild.
More information on omega-3s is available in the ODS (Office of Dietary Supplements) health professional fact sheet on omega-3s.
The soil concentration of selenium varies geographically around the world, affecting selenium status and resulting in endemic insufficiency and deficiency (Ref). A study comparing COVID-19 survival to regional selenium status during a major outbreak in China found survival was more likely in high-selenium regions (Ref). A study done during an outbreak in Germany found higher selenium and selenium-containing protein levels in COVID-19 infection survivors versus non-survivors (Ref).
Blood selenium levels have been noted to diminish in patients with critical illness, and lower levels are correlated with more severe illness and lower chance of survival (Ref). A meta-analysis of 19 randomized controlled trials found intravenous selenium supplementation in critically ill patients reduced total mortality (but not 28-day mortality) and shortened the length of hospital (but not intensive care unit) stay (Ref).
Studies have not evaluated melatonin supplementation during pregnancy and breastfeeding, but some research suggests that these supplements might inhibit ovarian function (Source). Therefore, some experts recommend that women who are pregnant or breastfeeding avoid taking melatonin.
Related: Nature's Bounty Melatonin 5 mg > One tablet before bedtime (Amazon)
7. Glutathione, NAC and COVID-19
N-acetylcysteine (NAC) is a precursor to glutathione. It is an antioxidant and increases glutathione levels in the body (Source). NAC has mucolytic activity, so it helps reduce respiratory mucus levels. Laboratory research suggests that NAC might boost immune system function and suppress viral replication. NAC also decreases levels of interleukin-6 and has other anti-inflammatory effects.
Much of the research on NAC has used an inhaled, liquid form of this compound. This form—which is classified as a drug, not a dietary supplement—is approved by the U.S. Food and Drug Administration (FDA) as a mucolytic agent and for decreasing respiratory secretion viscosity (Source). Products containing NAC are also sold as dietary supplements.
NAC and COVID-19
According to this paper (2021), SARS-CoV2 infection impairs the metabolism and redox function of cellular glutathione. According to the authors, NAC can prevent this damage and the role of NAC in COVID-19 therapy is worth investigating.
Studies published in ACS Infectious Disease (ACS Infect Dis. 2020) and Antioxidants proposed that glutathione plays a crucial role in the body's fight against the severe inflammatory response triggered by the SARS-CoV-2 virus. The research group in the ACS Infectious Disease study called it the “most likely cause of serious manifestations and deaths in COVID-19 patients.”
NAC inhibits cellular entry and replication of some respiratory viruses, assists in clearing thickened mucous from the airways, suppresses inflammatory signaling, and may help mitigate viral infection-induced cytokine storm (Ref).
In a paper on NAC for COVID-19, published in the October 2020 issue of Clinical Immunology titled “Therapeutic Blockade of Inflammation in Severe COVID-19 Infection With Intravenous N-acetylcysteine”, which is a case series report of 10 patients (including one with G6PD deficiency) given intravenous NAC. NAC elicited clinical improvement and markedly reduced inflammatory marker, CRP in all patients. NAC mechanism of action may involve the blockade of viral infection and the ensuing cytokine storm.
In a paper on NAC for COVID-19, published in the October 2020 issue of Clinical Immunology titled “Therapeutic Blockade of Inflammation in Severe COVID-19 Infection With Intravenous N-acetylcysteine”, which is a case series report of 10 patients (including one with G6PD deficiency) given intravenous NAC. NAC elicited clinical improvement and markedly reduced inflammatory marker, CRP in all patients. NAC mechanism of action may involve the blockade of viral infection and the ensuing cytokine storm.
Another paper from US researchers, titled "N-Acetylcysteine to Combat COVID-19: An Evidence Review", offers a thorough analysis of NAC and discusses its potential use for treatment of COVID-19.
Another study, "Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations and Death in COVID-19 Patients" was led by Dr Alexey Polonikov from Russia (ACS Infect Dis. 2020).
What he found was that the reactive-oxygen-species-to-glutathione ratio was able to predict the severity of COVID-19 and the patient’s outcome. When the patient had a low ROS-to-glutathione ratio, the patient had a very mild case. The fever disappeared on the fourth day without any treatment whatsoever.
When the ROS-to-glutathione ratio was high, the patient developed air hunger on the fourth day, experienced significant fever, hoarseness, myalgia and fatigue persisting for 13 days. A patient with even higher ROS and lower reduced glutathione had critical disease requiring hospitalisation for COVID-19-related pneumonia.
Foods that have a positive impact on glutathione production include cruciferous vegetables such as broccoli, green tea, curcumin, rosemary and milk thistle. Getting quality sleep may also help.
Different types of exercise can influence your levels as well. In one study, researchers enrolled 80 healthy but sedentary volunteers to measure the type of exercise that may have the greatest effect. They found that aerobic training in combination with circuit weight training showed the greatest benefit.
When the ROS-to-glutathione ratio was high, the patient developed air hunger on the fourth day, experienced significant fever, hoarseness, myalgia and fatigue persisting for 13 days. A patient with even higher ROS and lower reduced glutathione had critical disease requiring hospitalisation for COVID-19-related pneumonia.
In another publication on Respiratory Medicine Case Reports:
Two patients living in New York City (NYC) with a history of Lyme and tick-borne co-infections experienced a cough and dyspnea and demonstrated radiological findings consistent with novel coronavirus pneumonia (NCP). A trial of 2 g of PO or IV glutathione was used in both patients and improved their dyspnea within 1 h of use. Repeated use of both 2000 mg of PO and IV glutathione was effective in further relieving respiratory symptoms.
Two patients living in New York City (NYC) with a history of Lyme and tick-borne co-infections experienced a cough and dyspnea and demonstrated radiological findings consistent with novel coronavirus pneumonia (NCP). A trial of 2 g of PO or IV glutathione was used in both patients and improved their dyspnea within 1 h of use. Repeated use of both 2000 mg of PO and IV glutathione was effective in further relieving respiratory symptoms.
Different types of exercise can influence your levels as well. In one study, researchers enrolled 80 healthy but sedentary volunteers to measure the type of exercise that may have the greatest effect. They found that aerobic training in combination with circuit weight training showed the greatest benefit.
As of July 2021, more than 10 clinical trials are underway to assess the efficacy of NAC in the context of highly infectious respiratory viral infections.
What Is the Primary Cause of Severe COVID-19 Illness: Glutathione or Vitamin D Deficiency?
The hypothesis that vitamin D (VD) deficiency is responsible for severe manifestations and death in COVID-19 patients has been proposed and is actively being discussed by the scientific community.
Several studies reported that glutathione levels positively correlate with active vitamin D. (PubMed, PubMed)
Interestingly, a recent experimental study (PubMed) showed that Glutathione deficiency and the associated increased oxidative stress epigenetically alters vitamin D regulatory genes and, as a result, the suppressed gene expression decreases Vitamin D production, ultimately leading to a secondary deficiency of vitamin D. This study provides important information that glutathione is essential for the control of endogenous vitamin D production and demonstrates potential benefits of Glutathione treatment in reducing the deficiency of vitamin D. Taken together, these findings suggest that glutathione deficiency rather than vitamin D deficiency is a primary cause underlying biochemical abnormalities, including the decreased biosynthesis of vitamin D, and is responsible for serious manifestations and death in COVID-19 patients.
NAC (N-Acetyl Cysteine) vs Glutathione
N-acetyl L-cysteine (NAC), as a precursor of glutathione, helps to replenish intracellular glutathione, a vital cellular antioxidant. NAC has a low molecular weight and is well absorbed via oral administration as compared to glutathione.NAC may also protect against coagulation problems associated with COVID-19, as it counteracts hypercoagulation and breaks down blood clots.
Glutathione and Zinc
To improve your glutathione, you need zinc, and zinc in combination with hydroxychloroquine (a zinc ionophore or zinc transporter) has been shown effective in the treatment of COVID-19.
Glutathione and Molecular Hydrogen
One of the best ways to increase glutathione, though, is molecular hydrogen. Molecular hydrogen does so selectively and will not increase glutathione unnecessarily if you don’t need it. You can view Tyler LeBaron’s lecture on the details of how it does this in “How Molecular Hydrogen Can Help Your Immune System.”
Glutathione and Selenium
Selenium is also important, as some of the enzymes involved in glutathione production are selenium-dependent.
NB: NAC supplements are not available on Amazon US. You can buy NAC Supplements from Lazada Singapore.
8. Green Tea (EGCG)
Quercetin and EGCG act as zinc ionophores (J. Agric. Food Chem. 2014), the same mechanism of action that hydroxychloroquine has via helping zinc pass the cell wall where it might halt viral replication.
Epigallocatechin-gallate (EGCG) 200mg (prevention) or 400 mg (early treatment) 1 time a day (J. Agric. Food Chem. 2014) is part of the Zelenko protocol for prevention and early treatment of COVID-19. EGCG acts as a zinc ionophore and therefore needs to be combined with zinc.
The strong oxidative stress-reducing and anti-inflammatory effects of green tea catechins, including epigallocatechin gallate (EGCG), have been well established. A solution of green tea catechins was found to inactivate COVID-19 virus in the laboratory (Ref).
Other laboratory and computer models suggest tea catechins may inhibit viral infectivity and growth (Ref). It has been proposed that EGCG, due to its immune-modulating effect, could have a role in suppressing hyper-inflammation and preventing lung fibrosis in patients with severe acute viral respiratory illness (Ref).
EGCG (Green Tea Extract), Quercetin, Zinc, Vitamin C and D - Zelenko Prevention Protocol
Dr Zelenko's prevention protocol recommends the following for COVID-19 prevention for Low and Moderate Risk Patients:
2.1. Quercetin (Amazon) 500mg 1 time a day until a safe and efficacious vaccine becomes available. If Quercetin is unavailable, then use
3. Vitamin D3 5000 iu 1 time a day (Amazon)
EGCG (Green Tea Extract), Quercetin, Zinc, Vitamin C and D - Zelenko Treatment Protocol
Dr Zelenko's outpatient (over the counter options) 'treatment' protocol recommends the following for COVID-19 treatment for Low Risk Patients:
1. Elemental Zinc 50mg 1 time a day for 7 days (PubMed)
2.1. Quercetin (Amazon) 500mg 2 times a day for 7 days (PubMed) OR
2.2. Epigallocatechin-gallate (EGCG) 400mg 1 time a day for 7 days (J. Agric. Food Chem. 2014)
4. Vitamin C 1000mg 1 time a day for 7 days
9. Fish Oil (Omega-3 Fatty Acids) and Omega-6
Omega-3 fatty acids (omega-3s) are polyunsaturated fatty acids that are present in certain foods, such as flaxseed and fatty fish, as well as dietary supplements, such as those containing fish oil. Several different omega-3s exist, including alpha linolenic acid (ALA), but most scientific research focuses on the long-chain omega-3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). The main food sources of EPA and DHA are fatty fish and fish oil.Higher intakes and blood levels of EPA and DHA are associated with lower levels of inflammatory cytokines (Source). Omega-3s might also affect immune function by up-regulating the activity of macrophages, neutrophils, T cells, B cells, natural killer cells, and other immune cells.
Omega-3 Fatty Acids and COVID-19
This protection may have come from the effect EPA and DHA have on the body. An opinion paper published in June 2020 in the journal Frontiers in Physiology expounded on how "EPA and DHA supplementation can alter many biological pathways which may have a direct influence in the outcome of COVID-19."(Front. Physiol., 19 June 2020) The writers listed the many nutrients that play a key role in managing a cytokine storm and continued:
Omega-3 Fatty Acids are part of the I-Recover treatment protocol for Long Haul or Post-COVID syndrome, launched on June 16, 2021 by the FLCCC (Front Line COVID-19 Critical Care Alliance).
A pilot study (Jan 2021) suggests that patients with the most omega-3s in their system were 75% less likely to die from COVID-19. The pilot study was conducted using blood drawn from 100 patients treated for COVID-19 at the Cedars Sinai Medical Center in Los Angeles. The postulated mechanism of action is the well known anti inflammatory role of higher omega-3 levels, which may helped quell the so-called 'cytokine storm' observed in some severe and/or fatal COVID-19 cases.
This protection may have come from the effect EPA and DHA have on the body. An opinion paper published in June 2020 in the journal Frontiers in Physiology expounded on how "EPA and DHA supplementation can alter many biological pathways which may have a direct influence in the outcome of COVID-19."(Front. Physiol., 19 June 2020) The writers listed the many nutrients that play a key role in managing a cytokine storm and continued:
"Among these micronutrients, LC-PUFAs (long-chain polyunsaturated fatty acids) such as EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are noteworthy because of their direct influence in the immunological response to viral infections.
Among these complex immunomodulatory effects, interleukin-6 (IL-6) and interleukin-1ß (IL-1β)—because of the suspected central regulatory role in the "cytokine storm"—should be highlighted."
Accumulating evidence shows omega-3 fatty acids, administered orally or intravenously, may help control inflammation and improve outcomes in critically ill patients, including those with ARDS.489 A meta-analysis of 12 randomized controlled trials with a total of 1,280 critically ill patients with ARDS found supplementation with omega-3 fatty acids, in combination with gamma-linolenic acid (a less-inflammatory omega-6 fatty acid) and antioxidants, improved markers of lung function; however, only hourly administration, rather than large bolus intravenous dosing, was associated with reduced mortality. Although reductions in mechanical ventilation and length of stay in intensive care were seen, these effects did not reach statistical significance (Ref).
An observational study in 100 patients hospitalized with a severe acute viral respiratory illness found higher levels of EPA plus DHA were associated with lower mortality, though the effect was not statistically significant, possibly due to the small number of participants (Ref). During an outbreak of a severe viral respiratory infection, another study found countries with the highest intake of omega-3 fatty acids from marine sources had lower mortality rates than other regions of the world (Ref). The same research group used computer modeling to show how omega-3 fatty acids might bind to the highly infectious virus and interfere with its ability to enter cells (Ref).
That are more than a dozen studies on-going that examine the effect of EPA and/or DHA on the prevention of or lessening of symptoms of COVID-19.
Evidence suggests the omega-3 fats EPA and DHA affect biological pathways that may have direct influence in the outcome of COVID-19.
EPA and DHA have a direct influence in the immunological response to viral infections and can modulate immune response and function.
Animal-based omega-3 fats, especially DHA, also help prevent thrombosis (a blood clot within a blood vessel) by decreasing platelet aggregation. Hypercoagulation is another complication of severe COVID-19 infection that can have lethal consequences.
Omega-3 also lowers your risk of lung dysfunction, protects against lung damage and secondary bacterial infections, and improves mitochondrial function.
Research shows that by lowering triglycerides, the risk of developing a cytokine storm is diminished. Omega-3 supplementation is known to lower triglycerides, but krill oil does so more effectively than fish oil.
The British Rhinological Society's Guidelines for the Management of New Onset Loss of Sense of Smell During the COVID-19 Pandemic advises that that fish oil supplementation (2,000 mg of omega-3 fatty acids/day) may be beneficial when used in addition to standard treatment (olfactory training, oral steroids and steroid rinses) (Hopkins, Clin Otolaryngol 2020). This position is not based on a clinical trial of fish oil in COVID-19 patients but on limited animal and human research suggesting that omega-3 fatty acids may be beneficial for loss of smell due to olfactory nerve damage.
Doses of 2–15 g/day EPA and/or DHA might also increase bleeding time by reducing platelet aggregation (Source). However, according to the European Food Safety Authority (EFSA), long-term consumption of EPA and DHA supplements at combined doses of up to about 5 g/day appears to be safe for adults. EFSA noted that these doses have not been shown to cause bleeding problems or affect immune function, glucose homeostasis, or lipid peroxidation.
Commonly reported side effects of omega-3 supplements—including unpleasant taste, bad breath, heartburn, nausea, gastrointestinal discomfort, diarrhea, headache, and odoriferous sweat—are usually mild.
More information on omega-3s is available in the ODS (Office of Dietary Supplements) health professional fact sheet on omega-3s.
Related: Best Fish Oil Supplements 2021
10. B Vitamins and COVID-19
Thiamine (vitamin B1), a water-soluble B-complex vitamin, is rapidly depleted during times of metabolic stress, including severe illness. Thiamine deficiency is common in hospitalized patients, especially those with critical illness (Ref). Thiamine is needed for cellular energy production and helps regulate reduction-oxidation balance, immune function, nervous system function, and vascular function (Ref).
Thiamine, at 200 mg twice daily, reduced mortality in patients with septic shock and thiamine deficiency, and laboratory research suggests it may inhibit the hyper-inflammatory immune response that accompanies cytokine storm (Ref). It is a key therapeutic in the MATH+ protocol (methylprednisolone, ascorbic acid [vitamin C], thiamine, and heparin, plus other supportive nutrients and medications), a treatment strategy proposed for managing advanced stages of severe acute viral respiratory illness (Ref). Although high-quality clinical evidence is lacking, two US hospitals implementing the MATH+ protocol in patients with a severe acute viral respiratory illness reported mortality rates that were approximately one-quarter of those reported from other US hospitals using standard care (Ref).
In a study in Saudi Arabia (Al Sulaiman et al. Crit Care 2021), 738 critically ill COVID-19 patients from two centers were included in the study. The in-hospital death rate and 30-day death rate were significantly lower in the group that received thiamine as an adjunctive treatment (a therapy given in addition to standard therapy). In addition, the thiamine group also were less likely to have blood clot during ICU stay.
Another study of COVID-19 patients with severe symptoms found 26.3% among diabetics with COVID-19 were vitamin B1 deficient.
Adequate amounts of folate, vitamin B6 and vitamin B12 are also needed for your body to make the amino acid cysteine. N-acetyl cysteine (NAC) is a supplement form of cysteine. Consuming adequate cysteine and NAC is important for a variety of health reasons — including replenishing the most powerful antioxidant in your body, glutathione.
A study published in November 2020 from Singapore (CW Tan, Nutrition 2020), found that those who were started on a daily oral dose of vitamin D3 (1,000 IU), magnesium (150 mg) and vitamin B12 (500 mcg) within the first day of hospitalisation and continued up to 14 days were significantly less likely to require oxygen therapy and further intensive care.
A case series (published in September 2020) of 9 elderly COVID-19 patients treated with a combination of NMN, zinc, betaine and sodium chloride resulted in rapid improvement.
The topic 'B vitamins' is a complicated subject and that's probably why they are called 'B Complex'.
B vitamins may constitute a long list, but each one is important for different reasons. B vitamins are especially effective in boosting your immunity when you combine the foods containing them so they can all work together for maximum effect. These include vitamin B1 (thiamin), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid) and B7 (biotin).
B12, also known as cobalamin, is a powerful cold- and flu-fighting nutrient in your system, as is vitamin B6, another important, germ-combating vitamin that naturally benefits and strengthens your immune system and even protects against the damaging effects of air pollution.
Vitamin B9 and folic acid help repair tissues and aid in cell metabolism and immune support. They’re found in dark leafy greens, wild-caught, cold water fish like herring, mackerel, sardines, anchovies and wild-caught Alaskan salmon, and pastured, organic chicken.
B12, also known as cobalamin, is a powerful cold- and flu-fighting nutrient in your system, as is vitamin B6, another important, germ-combating vitamin that naturally benefits and strengthens your immune system and even protects against the damaging effects of air pollution.
Vitamin B9 and folic acid help repair tissues and aid in cell metabolism and immune support. They’re found in dark leafy greens, wild-caught, cold water fish like herring, mackerel, sardines, anchovies and wild-caught Alaskan salmon, and pastured, organic chicken.
Niacin or vitamin B3 is a precursor to nicotinamide adenine dinucleotide (NAD+). There are three main forms of niacin, which are dietary precursors to nicotinamide adenine dinucleotide (NAD). These are nicotinamide riboside, nicotinic acid and nicotinamide.
Nicotinamide adenine dinucleotide (NAD+) is an essential cofactor in all living cells that is involved in fundamental biological processes. NMN (Nicotinamide MonoNucleotide), is also another precursor to NAD.
Related: Niacin and COVID-19 - Is Niacin a Missing Piece of the COVID Puzzle?
11. Molecular Hydrogen
Molecular hydrogen has been tested in several registered clinical trials right now as a potential treatment option for COVID-19.
There have been a plethora of studies on hydrogen’s effects on inflammation, in particular in regulating/controlling inflammatory cytokines. For example:
Beyond the existing scientific studies that show a reason for excitement, hydrogen gas is also now being recommended in China as a therapy for individuals suffering from COVID-19, and there are very positive recorded anecdotal reports from patients.
The science behind the virus and potential treatment is, of course, far more complex than this, and we do not intend to simplify the situation whatsoever. Nonetheless, the potential here is interesting — especially when you factor in the safety factor of molecular hydrogen. We will have to see what happens as the science develops and the clinical trials are conducted, and we will update this article with more information as it becomes available.
- A group of scientists in China suggested that hydrogen-rich solution therapy may be a safe, reliable, and effective treatment for Multiple Organ Dysfunction Syndrome (MODS) induced by influenza and other viral infectious diseases (SOJ Microbiol Infect Dis. 2017).
- In a 2017 lab study published in the World Journal of Gastroenterology, “HRW (hydrogen rich water) treatment significantly reduced EtOH-induced increases in serum alanine amino transferase, aspartate aminotransferase, triglycerol and total cholesterol levels, hepatic lipid accumulation and inflammatory cytokines, including tumor necrosis factor-alpha (TNF-α) and interleukin (IL)-6.”
- Another study in 2013 stated “The serum levels of cytokines such as IL-10, TNF-α, IL-12p70, and GM-CSF of mice administered with HW (hydrogen water) was significantly reduced as compared to PW (placebo water) group.”
Beyond the existing scientific studies that show a reason for excitement, hydrogen gas is also now being recommended in China as a therapy for individuals suffering from COVID-19, and there are very positive recorded anecdotal reports from patients.
- The epidemiologist who discovered the SARS Coronavirus back in 2003, Dr. Zhong Nanshan, is now recommending H2 therapy for COVID-19 — you can watch the video where he does so here.
- Other individuals in the scientific community are talking about hydrogen as a possible treatment for COVID-19.
The first preliminary report on COVID-19 patients (n=90) from China has been published demonstrating that Hydrogen/Oxygen mixed gas inhalation has superior effects compared to Oxygen alone (Journal of Thoracic Disease. 2020).
12. Selenium
Selenium plays a role in immune cell function and activation through its incorporation into enzymes and other proteins. It also reduces infectivity, replication, and virulence of several respiratory viruses (Ref). Sodium selenite, a form often used in supplements, has been found to block an infectious respiratory virus from entering cells by interacting with its spike protein in the laboratory (Ref).Selenium works closely with vitamin E and cysteine to regulate oxidation and reduction balance and neutralize free radicals, and can help reduce inflammatory signaling by controlling oxidative stress (Ref). Poor selenium status may also increase the likelihood of induction of excess inflammation due to cytokine storm (Ref).
The soil concentration of selenium varies geographically around the world, affecting selenium status and resulting in endemic insufficiency and deficiency (Ref). A study comparing COVID-19 survival to regional selenium status during a major outbreak in China found survival was more likely in high-selenium regions (Ref). A study done during an outbreak in Germany found higher selenium and selenium-containing protein levels in COVID-19 infection survivors versus non-survivors (Ref).
Blood selenium levels have been noted to diminish in patients with critical illness, and lower levels are correlated with more severe illness and lower chance of survival (Ref). A meta-analysis of 19 randomized controlled trials found intravenous selenium supplementation in critically ill patients reduced total mortality (but not 28-day mortality) and shortened the length of hospital (but not intensive care unit) stay (Ref).
In a randomized controlled trial in 40 patients with ARDS, those who received sodium selenite intravenously for 10 days had increased glutathione levels, decreased inflammatory cytokine levels, and improved lung function compared with those who received saline (placebo). However, there were no differences in survival or intensive care unit stay (Ref).
13. Probiotics
Probiotics act mainly in the gastrointestinal tract (Source). They might improve immune function in several ways, including enhancing gut barrier function, increasing immunoglobulin production, inhibiting viral replication, and enhancing the phagocytic activity of white blood cells. However, the mechanisms of their potential effects on immune function are unclear. In addition, research findings for one probiotic strain cannot be extrapolated to others.
Through the mesenteric lymphatic system, intact bacteria and their metabolites enter the circulation and influence the lung immune response (gut/lung axis). Through this way intestinal metabolites, mainly produced by bacterial fermentation of dietary fiber, such as short-chain fatty acids (SCFAs), significantly influence local gut immunity but also distant organs. SCFAs derived from gut are able to suppress lung inflammation (Ref). Dendritic cells (DCs), the antigen-presenting cells of the immune system, stimulate T-cells subpopulations in mesenteric lymph nodes and gut lymphatic tissue to produce regulatory cytokines. After airways immune-stimulation, these T-cells move from the gut to the respiratory system, providing protection and stimulating an anti-inflammatory response. In fact, gut microbiota rebalancing has been shown to reduce ventilator-associated enteritis and pneumonia (Ref).
Altered bacterial balance (dysbiosis) causes the translocation of cytokines, endotoxins and microbial metabolites in the general circulation to other organs, such as the lung. Conversely, respiratory inflammation (due to many causes, e.g., respiratory viral infections due to COVID-19 virus), causes local dysbiosis and, in turn, the translocation of microbial metabolites and toxins to other organs, such as the gut (below).
Physiological changes in the human microbiota with age leads to a “physiological dysbiosis”, with less diversification in microbial composition, aggravated in case of comorbidity (hypertension, diabetes, chronic inflammatory bowel diseases, etc.) (Ref). Therefore, to establish the condition of eubiosis (healthy condition), “good” bacteria are required. The concept of probiotics as a food with positive effects was firstly used by Parker RB in 1974 and then recognized by the Food and Agriculture Organization (FAO), and more recently by the Word Health Organization (WHO) (Ref).
Multiple randomized controlled trials and several meta-analyses have shown probiotics reduce the risk of acute respiratory tract infections (eg, colds and flu) (Ref).
Self-reported use of probiotic supplements more than three times per week for at least 3 months among 372,720 U.K. residents aged 16 to 90 years was associated with a 14% lower risk of SARS-CoV-2 infection after adjustment for potential confounders (Source). Findings were similar for 45,757 individuals in the United States and for 27,373 participants in Sweden.
Another clinical study in Italy showed a better prognosis in 28 of 70 symptomatic patients taking probiotics (L. acidophilus DSM 32241, L. helveticus DSM 32242, L. paracasei DSM 32243, L. plantarum DSM 32244, L. brevis DSM 27961, B. lactis DSM 32246, B. lactis DSM 32247, 2400 billion bacteria per day), reducing the risk of admission in ICU. All these actions would be useful in reducing SARS-CoV-2 dissemination in the respiratory tract and gut, reinforcing both anti-inflammatory responses and immune defenses (Ref).
Recently, several peer-reviewed reports of clinical experiences, preclinical studies, small, open clinical trials, case series, and clinical hypotheses have suggested that certain immune-modulating probiotic strains, such as L. rhamnosus CRL-1505 (Ref), Streptococcus salivarius K12 (Ref), L. plantarum LP01 (Ref), and B. lactis BS01 (Ref) may confer protection against respiratory viral infections and/or subsequent inflammatory sequela.
The first quadrupled blinded randomised controlled trial (MedRxiv May 2021) on a novel probiotic formulation demonstrated that complete remission on day 30 was boosted from 28% to 53%.
Numerous clinical trials to investigate the usefulness of probiotics in treating severe acute viral respiratory infections have been registered since early 2020, and many are currently underway.
More information on probiotics is available in the ODS health professional fact sheet on probiotics.
14. Lactoferrin
Lactoferrin is an iron-binding protein made by cells such as those in secretory glands and activated neutrophils (a type of immune cell). It is found in most bodily fluids, including tears and breast milk, and lactoferrin derived from bovine whey is frequently used in supplements (Ref). Lactoferrin is an immune modulator, capable of enhancing antimicrobial immune activity while reducing inflammation, and has exhibited a broad spectrum of activity against bacteria, fungi, protozoa, and viruses (Ref). Laboratory research also suggested lactoferrin may inhibit entry of a highly infectious respiratory virus into cells by blocking its interactions with cell membrane components (Ref).Lactoferrin may slow pathogen multiplication through its iron binding capacity. While iron is required for DNA replication and energy production, the presence of excess iron increases free radical generation, stimulates inflammatory processes, and exacerbates viral infection by promoting increased viral replication (Ref). Furthermore, patients with a severe acute viral respiratory infection have been found to have elevated levels of ferritin, and these levels correlated with increased risk of death (Ref). In its iron-free state (apolactoferrin), lactoferrin can sequester pro-oxidant free iron, lowering oxidative stress and suppressing the growth of pathogens, and possibly mitigating the serious complications of infection (Ref).
In a pilot trial, 75 patients who tested positive for an acute viral respiratory tract infection were treated at home with a liposomal preparation of a combination of 32 mg bovine lactoferrin with 12 mg vitamin C, with or without 10 mg liposomal zinc, four to six times daily for 10 days. In addition, lactoferrin nasal drops, mouth spray, and aerosol were used as needed by participants with headaches, loss of sense of smell and taste, nasal congestion, dry cough, or difficulty breathing. After 48 hours, all symptoms had diminished except loss of smell and taste, and by day five, all infected participants recovered from their illness with only loss of smell and taste remaining as residual symptoms (Ref).
15. Astaxanthin
The paper (SSRN) “COVID-19: Potential of Microalgae Derived Natural Astaxanthin as Adjunctive Supplement in Alleviating Cytokine Storm,” published April 21, 2020, on the research library website SSRN, addresses the use of astaxanthin, a potent antioxidant supplement derived from microalgae. The full paper is downloadable from the link.As explained in this paper, astaxanthin has a very unique molecular structure that allows it to penetrate the bilayer membrane of cells. The ability to quench reactive oxygen species (ROS) and free radicals in both the inner and outer layers of the cellular membrane allows it to provide superior protection against oxidative stress, compared to other antioxidants.
Vitamin E and beta-carotene, for example, only work in the inner side of the membrane, and vitamin C only works on the outer side.
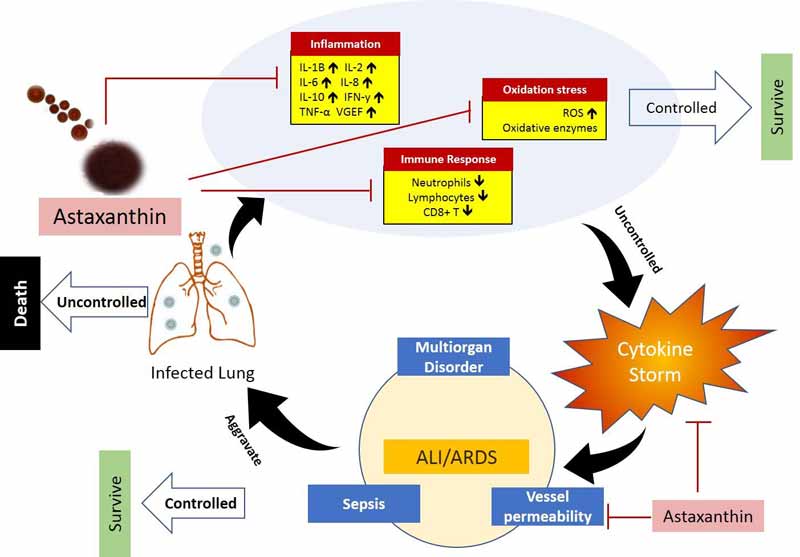
In short, astaxanthin ticks many important boxes when it comes to ameliorating COVID-19, including immune response regulation and the enhancement of both cell-mediated and humoral immune responses, as well as the simultaneous protection against oxidative damage and inflammation.
Conclusion
Macronutrients and micronutrients are essential to a human body, there are no ifs and buts about it. Optimizing your immune system is critical to improve your health whether there is a pandemic or not.Optimizing your immune system with diet and lifestyle changes are critical to improving your health and to decrease your risk with COVID-19. However, therapeutics, vaccines and other physical strategies such as social distancing and mask wearing are also needed in order to protect yourself and your loved ones. It doesn't have to be an 'either or' situation. Combination strategies are normally more effective.
Nutritional supplements are meant to tip the scales in favour of you in terms of your immune system and to improve your probability of a smooth recovery, if at all you do get COVID-19. You still need to follow the advice given by CDC, WHO and your local authority in terms of local guidelines.






.png)




Comments
Post a Comment