Essential Guide to Chronic Kidney Disease: Symptoms, Causes, Treatments and Natural Approaches
Chronic kidney disease (CKD) is a progressive disorder of the kidney that is also known as chronic kidney failure. Affecting over 800 million people worldwide, CKD is characterized by a slow loss of kidney function.
CKD is the eighth leading cause of death worldwide.
What Are the Symptoms and Early Signs of Chronic Kidney Disease?
Symptoms of CKD occur over time and become more severe as the illness progresses. When kidneys are damaged, and their function deteriorates, patients experience a buildup of fluid, body waste, and frequently an electrolyte imbalance because of the kidneys’ inability to filter blood.
When kidneys begin to lose their function, the following symptoms may appear:
- Fatigue and weakness
- Tiredness
- Loss of appetite
- Shortness of breath due to fluid buildup in the lungs
- Chest pain due to fluid buildup around the heart’s lining
- Vomiting
- Nausea
- Hypertension
- Darkening of the skin
- Muscle cramps
- Problems sleeping
- Swelling in the ankles or feet
- Urinary frequency
- Trouble concentrating
- Itchy or dry skin
Because the symptoms of kidney disease are common and could also be caused by other conditions, it can be easy to overlook the seriousness of these signs. It’s essential to notify your provider of any of the above-listed symptoms to assist with early detection and help prevent irreversible damage to your kidneys.
What Causes Chronic Kidney Disease?
Although the cause of CKD is not always known, high blood pressure and diabetes are among the most common causes.
High Blood Pressure
When blood pressure is too high, the blood vessels in the kidneys narrow, eventually damaging the vessels and causing a reduction in the amount of blood flowing to the kidneys. When this occurs, the kidneys cannot appropriately remove the extra fluid and waste from the body. This fluid buildup in the blood vessels must be removed, and it may raise blood pressure if the kidneys cannot remove it.
One in 5 American adults (20 percent) with high blood pressure may also suffer from CKD.
Diabetes
CKD is commonly linked to diabetes. Around 1 in 3 adults with diabetes also suffers from CKD.
Similar to high blood pressure, diabetes can cause kidney damage to the point that they are unable to filter out extra fluid and waste. This happens when a person has too much glucose (sugar) in their blood. Type 1 or Type 2 diabetes can cause kidney disease.
Kidney disease caused by diabetes is referred to as diabetic kidney disease. When the condition presents itself, a protein in the urine called albumin is usually the first indicator to surface.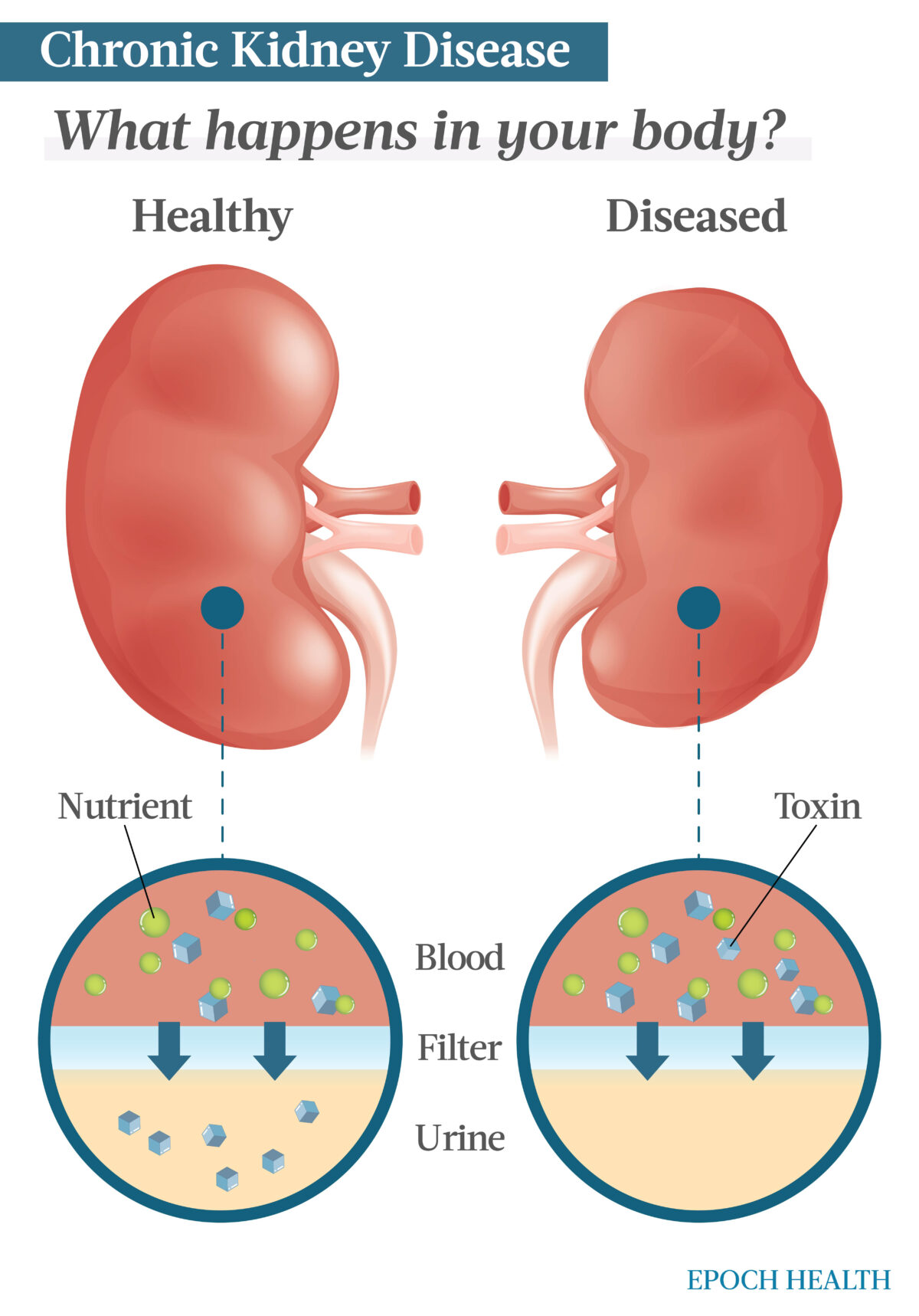
Kidney disease is the result of the kidneys not being able to properly filter waste from the body. It is most often caused by hypertension or diabetes. (The Epoch Times)
Other Conditions
Aside from diabetes and high blood pressure, many other conditions have been identified as potential causes of CKD.
- Lupus nephritis: This is a kidney disease caused by an autoimmune disease, systemic lupus erythematosus (SLE). Lupus-caused kidney disease may eventually lead to kidney failure.
- Kidney infection: Also known as pyelonephritis, this type of urinary tract infection begins in the urethra or bladder and can eventually infect one or both kidneys. This condition requires immediate medical treatment to avoid permanent kidney damage.
- Renal artery stenosis: Renal artery stenosis occurs when one or more arteries carrying blood to your kidneys narrow in diameter. These narrowed arteries reduce the amount of oxygen-rich blood flowing to the kidneys. When blood flow is reduced, kidney tissue may become damaged and increase blood pressure.
- Genetic disorder: Genetic disorders are not preventable, but medications can help manage some of them. Examples of genetic disorders include polycystic kidney disease, nephropathic cystinosis, and Alport syndrome.
- OTC drugs: Consuming large amounts of over-the-counter medications such as ibuprofen, naproxen, and aspirin can damage your kidneys.
- Antibiotics: These can be hazardous if not taken as prescribed. Patients with kidney disease should only take medications ordered by their physicians.
- Heavy drinking: Excessive drinking can damage both your kidneys and liver. Alcoholics are at a higher risk of developing kidney failure.
- Street drugs: Heroin, cocaine, and amphetamines may injure the kidneys.
- Contrast dyes: Some imaging tests, such as CT scans, that use contrast dye can cause severe kidney issues. This is referred to as contrast-induced nephropathy (CIN). It’s estimated that 1 to 3 percent of people who receive contrast dye experience changes in kidney function. Anyone can get CIN, but those with kidney disease are at greater risk of developing complications.
- IgA vasculitis: This disorder causes antibody immunoglobulin A to gather in small blood vessels, causing them to become inflamed and leak. Some patients develop problems with their joints, gastrointestinal tract, and kidneys.
- Glomerulonephritis (IgA nephropathy): IgA nephropathy, or Berger’s disease, is among a group of conditions called glomerulonephritis. IgA nephropathy is a kidney disorder that occurs when immunoglobulin A collects in the kidneys. Over time, this buildup causes inflammation that can decrease the kidneys’ ability to filter waste. It is progressive and may result in kidney failure.
- Autoimmune disorders: An autoimmune disorder attacks the body’s own organs and cells. An example would be anti-GBM (Goodpasture’s) disease, which attacks the kidneys and lungs.
- Heavy metal poisoning: Lead poisoning is a serious health condition that can lead to kidney and other diseases.
- Hemolytic uremic syndrome (HUS): This disorder occurs when small blood vessels in the kidneys become inflamed and damaged. Clots may form when the kidneys become damaged and lead to kidney failure. HUS is most common among young children.
What Are the Stages of Chronic Kidney Disease?
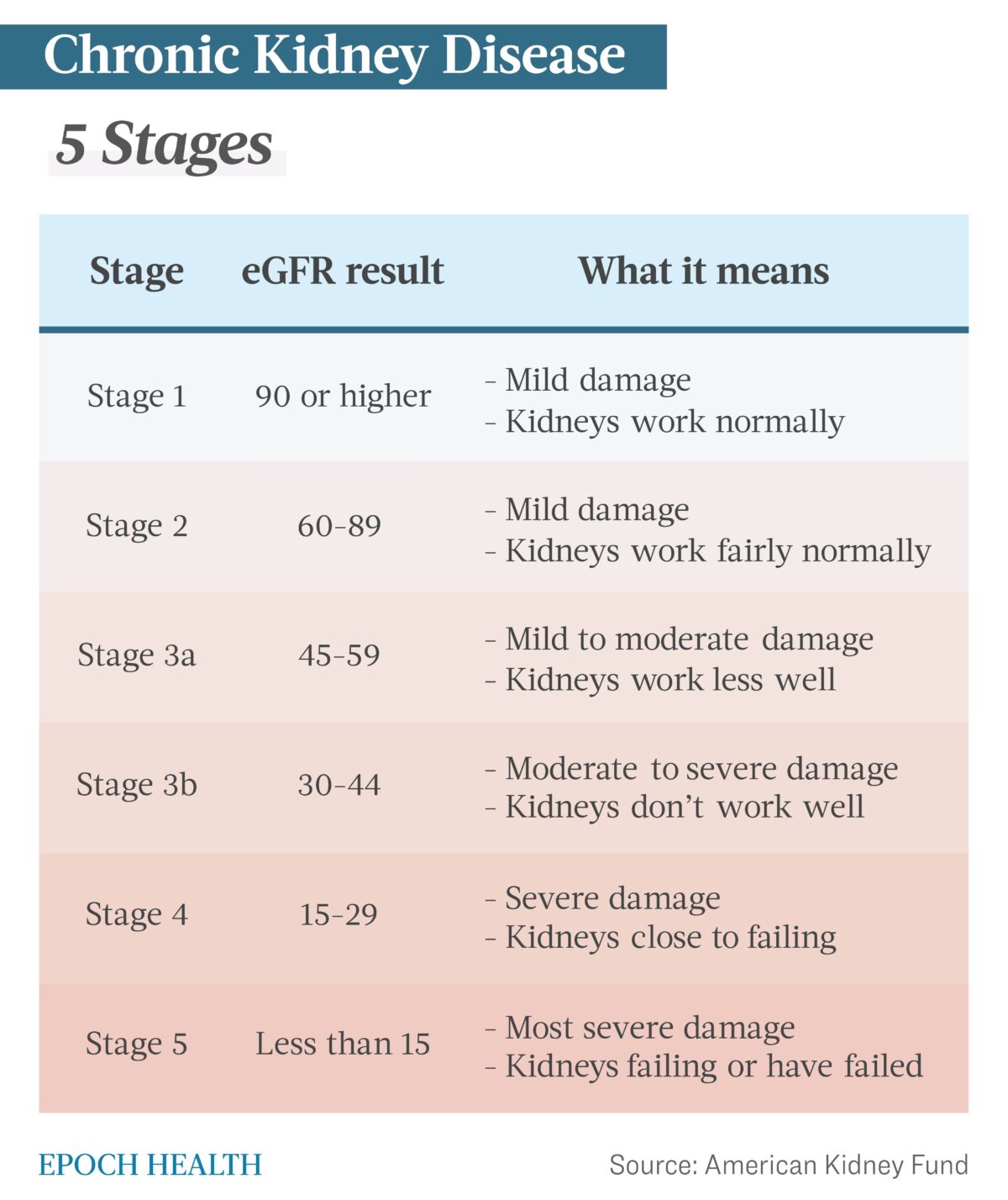
CKD is characterized by five stages. These are determined by the glomerular filtration rate (GFR) and estimated glomerular filtration rate (eGFR). GFR indicates the blood flow rate through the kidneys, while eGFR is a calculated number using a single blood test for creatinine. These tests measure the level of kidney function to determine the stage of the disease. Each increase in stage number reflects disease progression and further decline of kidney function.
Stage 1
These patients have a normal eGFR score of 90 or greater and mild kidney damage. At this stage, the kidneys are working well, and there may not be any noticeable symptoms, but signs like protein in the urine may be present.
Stage 2
Patients have an eGFR score between 60 and 89 with mild kidney damage. Kidneys are still working well for the most part, and there may still be no noticeable symptoms. However, signs such as protein in the urine or kidney damage may appear.
Stage 3
Stage 3 patients have an eGFR score between 30 and 59 with mild to moderate kidney damage. Kidneys are not working well and cannot appropriately filter fluid and waste. Excess fluid buildup may cause additional health problems such as hypertension. Symptoms such as swelling in the hands and feet, weakness, and fatigue are present.
Patients are categorized by two substages based on their eGFR results:
- Stage 3a: eGFR between 45 and 59
- Stage 3b: eGFR between 30 and 44
Patients compliant with treatment and adhering to healthy lifestyle changes may not progress to stages 4 or 5.
Stage 4
These patients have an eGFR score between 15 and 29 with moderate to severe kidney damage. This is the last stage before kidney failure. Kidneys do not work well and cannot filter excess fluid and waste. As a result, the patient is at risk of hypertension and heart disease. Symptoms such as lower back pain and swelling in the hands and feet appear.
Stage 5
Stage 5 patients have an eGFR of less than 15 and severe kidney damage. Kidneys are near failure or have already stopped functioning. When the kidneys have stopped filtering, waste builds up in the body, causing patients to become extremely sick and develop other health conditions. Treatment options at this time include dialysis or a kidney transplant.
Who Is More Likely to Develop Chronic Kidney Disease?
Many factors can increase the risk of developing CKD, including race. However, the main reason for increased risk in these populations is due to a high prevalence of hypertension and diabetes. The following types of people are at risk:
- Diabetics
- Those with high blood pressure
- Those with abnormal kidney function caused by other conditions
- Those who take a lot of medication, including OTC medications
- African Americans. This population accounts for 35 percent of Americans suffering from kidney failure. High blood pressure and diabetes are the leading causes of kidney failure in African Americans.
- Hispanics. The number of Hispanics diagnosed with CKD rises yearly, having grown by over 70 percent since 2000. Compared to non-Hispanics, Hispanics are approximately 1.3 times more likely to be diagnosed with kidney failure.
- American Indians. Compared to whites, American Indians are approximately 1.2 times more likely to be diagnosed with kidney failure. Diabetes is the leading cause of kidney failure in this group.
- Smokers
- Obese people
- Women. Research shows that women have a higher prevalence of CKD than men, but men are more likely to progress to complete kidney failure.
- Older people. CKD is often seen in adults aged 65 years and older.
- Those with a family history of kidney disease
What Are the Tests for Chronic Kidney Disease?
A health care provider may order one or more tests to evaluate, assess, and stage a patient for chronic kidney disease. Sometimes, a biopsy containing kidney cells may be recommended to determine the cause of your problem. A biopsy is performed under local anesthetic and then sent to the lab for study. In addition, an ultrasound may be used to determine the size and structure of your kidney. Your doctor may also order a lab test.
Laboratory tests
- Glomerular filtration rate (GFR): This blood test examines how well your kidneys filter blood. Most people with a score of 15 or lower will need dialysis or a kidney transplant.
- Kidney function tests: These blood tests study your body’s level of waste products like urea and creatinine.
- Urine tests: A urine test checks for the albumin protein. Albumin is passed into the urine when the kidneys are damaged.
What Are the Complications of Chronic Kidney Disease?
Numerous complications associated with CKD can impact nearly every part of the body. Complications may include:
- Anemia.
- Pericarditis.
- Heart disease.
- High potassium levels interfering with the heart’s normal electrical conduction and preventing the heart from beating effectively.
- Fluid retention leading to high blood pressure, fluid in the lungs, and swelling in the arms and legs.
- Weak bones leading to fractures.
- Pregnancy complications for mother and fetus.
- Damage to the central nervous system leading to personality changes, difficulty concentrating, and seizures.
- Decreased immune response, making patients more susceptible to infection.
- Erectile dysfunction, reduced fertility, and decreased sex drive.
- Irreversible kidney damage requiring dialysis or kidney transplant for survival.
What Are the Treatments for Chronic Kidney Disease?
Treatment recommendations for CKD depend on its type, stage, and cause. Some types of the disease can be treated, though CKD is often incurable.
Your physician will treat the disease’s cause and control complications to improve your quality of life. Treatment methods may include:
- Diet recommendations: Your physician may recommend low-sodium and low-protein diets. Low salt intake will help lower blood pressure and protein in the urine. Low-protein diets minimize waste buildup in your blood. Your doctor may also suggest increasing fruit and vegetable consumption. Their high nutrient content is beneficial to kidney health.
- Calcium and vitamin D supplements: Calcium and vitamin D supplements may help prevent your bones from weakening and lower your fracture risk. You might also take medication known as a phosphate binder to reduce the amount of phosphate in your blood and protect your blood vessels from calcium-deposit damage (calcification).
Medications
- Statins: Your physician may prescribe these to lower your cholesterol. CKD patients frequently experience high levels of bad cholesterol associated with heart disease. These medications include atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin.
- Diabetes medication: Diabetics may require a prescription to manage their blood sugar.
- Blood pressure medication: Because high blood pressure is a leading cause of kidney disease and other conditions, your physician will prescribe medication to manage your blood pressure if it’s elevated. These medications include benazepril, captopril, enalapril, lisinopril, and fosinopril.
- Medications to relieve swelling: People with chronic kidney disease often retain fluid, causing swelling, specifically in the legs. Your physician may prescribe a diuretic, or water pill, to help maintain blood pressure and reduce fluid retention. Examples of these medications include furosemide, bumetanide, and ethacrynic acid.
- Anemia medication: For anemia, your physician may recommend hormone supplements called erythropoietin to relieve fatigue and anemia-induced weakness. Erythropoietin is occasionally supplemented with iron to help with red blood cell production.
End-Stage Kidney Disease
There are no cures for some types of CKD, and people with end-stage disease may require dialysis or a kidney transplant.
- Dialysis: Dialysis may be needed when kidney damage is severe, and the kidneys can no longer remove extra fluid and waste buildup from your body. During peritoneal dialysis treatments, solution is inserted into the abdominal cavity to absorb excess fluids and waste. When hemodialysis is performed, a machine removes excess fluids and waste from your blood.
- Kidney transplant: This involves surgically replacing your diseased kidney with a healthy one from a compatible donor compatible. Donors may be living or deceased.
Some patients choose not to undergo dialysis or a kidney transplant. Instead, conservative measures, such as palliative and comfort care, are used when this choice is made.
How Does Mindset Affect Chronic Kidney Disease?
Patients living with CKD experience both physical and psychological effects (pdf). Managing mental health is as important as treating your physical well-being. It’s common for dialysis patients to be angry, frustrated, and feel like they have lost control over their bodies and life. This can often lead to anxiety, depression, difficulty sleeping, and other psychological challenges.
While we can’t help how we feel, we can control how we react and respond to those feelings. Staying positive can make a huge difference in your overall outlook and the happiness you experience in daily life. The following tips may help you maintain a positive and healthy mindset:
- Consider spirituality: Depending on your faith, spirituality might include believing in a higher power, visiting a place of worship, prayer, or meditation.
- Get support: Having a support system is extremely important. This could include family, friends, your spouse, preacher, co-worker, or anyone with whom you are comfortable sharing your thoughts and feelings. Aside from having someone who can listen to your fears and feelings, having another person’s support can lift you emotionally.
- Maintain self-care: Taking time to care for yourself may help you cope with the daily challenges of kidney disease. Choosing a healthy lifestyle that includes socializing, exercise, and a healthy diet is crucial to maintaining physical and mental well-being. It’s also critical to take your medications as prescribed by your physician.
- Set goals: Be purposeful. Give yourself something to focus on and strive for. For example, join support groups, get involved in your children’s school activities, or volunteer at your local animal shelter. Regardless of what type of group or activity you join, “giving back” will help you feel part of something and boost your mood and mindset.
- Seek professional help: Getting professional help, individually or in a group setting, can be beneficial. Negative feelings are normal when going through difficult times. Speaking with others facing the same challenges can help. It’s also helpful to talk to a physician openly and honestly about your feelings and allow him or her to determine if you might benefit from medication or therapy.
- Stay positive: Take one day at a time and try not to dwell on issues you cannot control. Accept help from others when you need it and engage with your family, friends, and support group.
What Are the Natural Approaches to Chronic Kidney Disease?
While kidney damage can’t be repaired once it’s occurred, a few natural approaches can improve your health. Kidney disease is a complex condition where special dietary restrictions and an exercise plan might help improve kidney function and overall health. Physical activity helps keep your kidneys healthy by supporting and maintaining weight loss and helping control blood pressure. Aim for getting at least 30 minutes of aerobic exercise most days of the week. These activities might include swimming, dancing, walking, hiking, etc.
Maintaining a proper diet is essential, too. Dietary recommendations might include the following:
- Low-potassium foods: Foods containing high potassium levels, such as potatoes, bananas, oranges, and tomatoes, may harm patients with kidney disease. Instead, select lower-potassium foods like carrots, cabbage, green beans, strawberries, and grapes.
- Low-salt foods: Reduce the amount of sodium you eat by steering clear of foods with added salt. These include frozen dinners, convenience foods, fast foods, and canned soups. There is also added salt in canned vegetables, salty snack foods, and processed meats and cheese.
- Lower-protein foods: Restrict the amount of protein you eat. Incorporate low-protein foods like fruits, vegetables, and whole grains. Avoid high-protein foods like eggs, milk, cheese, lean meats, and beans.
Vitamins and Supplements
Your physician may recommend supplements to ensure sufficient levels of certain nutrients. Recommendations may include:
- Iron: Iron helps your body produce red blood cells and may be prescribed if you have anemia. The iron must be taken as directed by your provider. Too much can cause adverse effects.
- B vitamins: B6, B12, thiamin, folic acid, and many other B vitamins are found in whole grains, eggs, mushrooms, meats, and bananas. Every B vitamin has its unique job; however, some supplements contain several B vitamins in one dose. A B vitamin complex may be recommended if you are anemic.
- Vitamin D: Vitamin D is essential for healthy bones and kidneys. Your provider may recommend a supplement if you are deficient in this vitamin.
- Omega-3s: These fatty acids are commonly recommended for people with coronary artery disease, heart failure, and many other conditions. Omega-3s, especially seafood-derived, may help lower blood pressure and reduce inflammation. Omega-3s can be found in oily fish such as salmon, mackerel, herring, anchovies, sardines, halibut, rainbow trout, and tuna.
- Sodium bicarbonate: Sodium bicarbonate offers many health benefits, especially for kidney disease patients, as it may slow the decline of kidney function. If you use it to make a “bicarb soda,” use pharmaceutical-grade sodium bicarbonate and not simple baking soda. However, not every CKD should take sodium bicarbonate, so only take it or sodium citrate pills if your health care provider recommends them.
Herbal Supplements
While studies indicate certain herbs and medicinal plants could be effective in mitigating CKD, it is always recommended to speak to your physician or a professional integrative or traditional Chinese medicine (TCM) health care provider before starting any regimen. Herbal medicines can undoubtedly benefit the kidneys, but they should be used cautiously in kidney disease patients to avoid overstimulating the kidneys. Kidney Coach has several home remedies that may help slow or stop the progression of CKD, though none is proven to work.
How Can I Prevent Chronic Kidney Disease?
CKD can potentially be prevented by controlling risk factors. If you have an increased risk of developing the disease, getting routinely checked for CKD is essential. You should also be assessed yearly if you have already been diagnosed with diabetes.
To keep your kidneys healthy and potentially prevent CKD, it’s essential to reduce your risk factors by doing the following:
- Maintain a healthy weight: Being overweight can increase the risk of developing high blood pressure and diabetes, the two leading causes of kidney disease. However, carrying extra weight can also directly affect your kidneys by forcing them to work harder to filter waste from the body. Gradually, this extra work will increase the risk of developing kidney disease.
- Increase physical activity: Most patients with kidney disease have been identified as “inactive with reduced physical functioning and performance.” Physical activity has been proven to improve physical function, performance, and blood pressure, control lipid profiles, and improve mental health.
- Quit smoking: Smoking slows blood flow to organs, including the kidneys, which can worsen kidney disease. This is equally detrimental to diabetic patients. When blood flow to your feet slows, sores may develop, and infections become more difficult to heal. It may also negatively affect the medications used to treat blood pressure.
- Monitor and manage the “3 highs”: Cholesterol, blood sugar, and blood pressure contribute to your heart disease and stroke risk. Among diabetics and those with high blood pressure, managing blood pressure and blood sugar management can lower the risk of developing CKD.
- Take medication: Keep up with medications as prescribed by your provider.
- Reduce your salt intake: Patients with CKD should keep low-salt diets. Less than one teaspoonful of salt per day is recommended.
- Consume more fruit and vegetables: Research suggests that a low intake of vegetables and fruits is linked to a higher probability of Americans developing kidney failure. Plant-rich diets can help prevent kidney failure and end-stage kidney disease. However, as kidney disease progresses, you may need to reduce the amount of certain fruits and vegetables to limit your phosphorus and potassium intake.
Medically reviewed by Beverly Timerding, MD.
Related: Chronic Kidney Disease (CKD) Diet


.png)
.png)


.png)

Comments
Post a Comment