Essential Guide to Colorectal Cancer: Symptoms, Causes, Treatments and Natural Approaches
Colorectal cancer is the third most diagnosed cancer in both men and women in the United States. While overall incidence rates seem to be dropping, rates in people under 50 have increased by 1 to 2 percent yearly since the mid-1990s. In addition, colorectal cancer is responsible for the second leading cause of cancer-related deaths when fatality numbers for both men and women are combined.
Part of the challenge of diagnosing colorectal cancer is that it often does not present symptoms until it has spread. Once symptoms present, gastrointestinal (GI) tests are often completed to rule out other complications or causes.
The good news is that colorectal cancer’s five-year relative survival rate is around 91 percent for localized cancers, meaning the cancer was caught early and did not spread to additional areas. If the cancer goes undetected and spreads to other areas of the body, these rates decline.
What Are the Common Types of Colorectal Cancer?
There are several different types of colorectal cancer. All occur due to uncontrollable cell growth in the tissue of the colon or rectum, which can spread elsewhere in the body. Some types of colorectal cancer seem to develop due to genetic predisposition or family history, whereas others do not show a genetic link.
- Adenocarcinoma: This accounts for about 95 percent of colorectal cancer cases and begins in the cells of the colon and rectum, responsible for secreting proteins that lubricate this part of the digestive tract. There are several layers of the colon’s wall, including a mucosa and submucosa layer, filled with the cells most commonly affected by these adenocarcinomas.
The other roughly 5 percent of colorectal cancers are comprised of the following:
- Gastrointestinal stromal tumor (GIST): More than half of these begin in the stomach, and most others begin in the small intestine, though they can occur anywhere in the GI tract. It is a rare tumor and constitutes about 0.1 percent of all colorectal cancers, resulting from the uncontrolled growth of specialized cells that normally act as nerve cells stimulating the bowel muscle. It rarely forms in the colon, and some are benign.
- Carcinoid tumors: These are rare types of colorectal cancer and typically form in the GI tract’s lining.
- Lymphoma: This type of colon cancer begins in the lymph nodes and affects the colon and GI tract. A rarer form of colorectal cancer, it affects only about 0.5 percent of GI lymphoma cases.
- Squamous cell tumor: This type of cancer is rare, making up only 1 percent of colorectal cases. It typically presents at a later stage and has a poor prognosis.
- Leiomyosarcoma: This rare cancer forms in smooth muscle connective tissue, including the anus.
What Are the Symptoms and Early Signs of Colorectal Cancer?
Colorectal cancer does not typically present with symptoms in earlier stages, making it more difficult to detect.
As colorectal cancer progresses, the following symptoms are common:
- Blood in the stool.
- Rectal bleeding (persistent and often accompanied by pain).
- Changes in bowel movements (i.e., constipation, diarrhea, changes in size or frequency).
- Abdominal pain (stomach cramps).
- Nausea or vomiting.
- Anemia.
- Unexplained weight loss.
Because many medical conditions can cause many of these symptoms, it is essential to consult a doctor if you begin to experience any to rule out other causes.
What Causes Colorectal Cancer?
The precise cause of colorectal cancer is unknown, but several factors are believed to be involved, one being polyps.
Many people have polyps, small groupings of cells, in the lining of their colons. Most polyps are harmless; however, some can develop into colorectal cancer. These are known as neoplastic polyps. Polyps may develop due to gene expression changes or dietary and lifestyle habits. Because polyps don’t typically present with symptoms, regular screening is important for detection.
What Are the Mechanisms Behind Colorectal Cancer?
Similarly to all cancers, colorectal cancer occurs when cells proliferate uncontrollably. The cells in the colon and rectum will continue to divide at an unnatural rate until they develop into a cancerous tumor.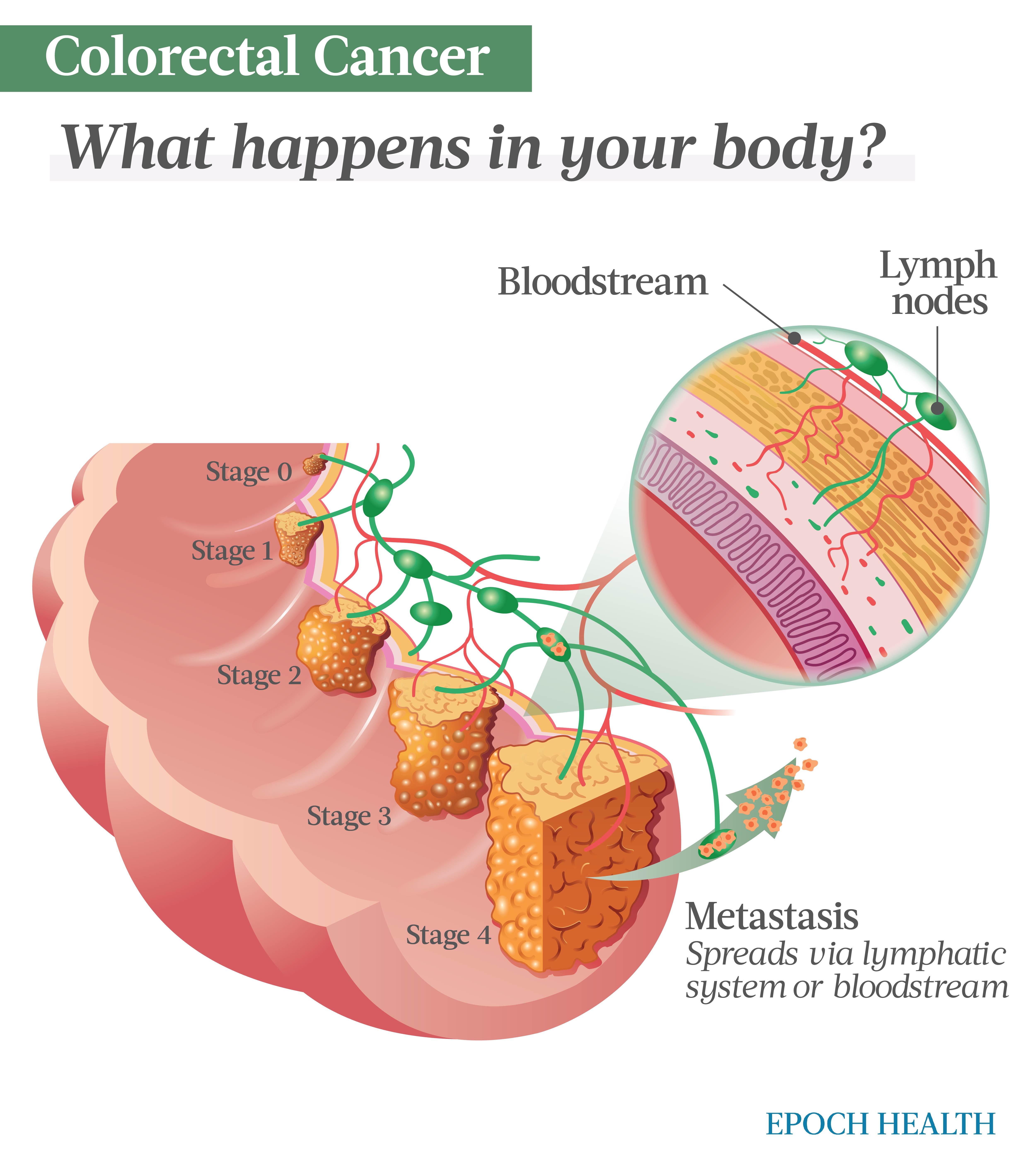
Colorectal cancer occurs when cancer cells divide uncontrollably in the colon or rectum, eventually developing into a tumor. (The Epoch Times)
Who Is More Likely to Develop Colorectal Cancer?
Both genetics and modifiable factors play a role in colorectal cancer risk. While further research is needed to understand why those with first-degree relatives who have had colorectal cancer are at a higher risk, there is an undeniable correlation, with an estimated heritable component of around 35 percent. These familial cancers seem to develop without any other known cause. Screening is recommended earlier in life for individuals whose relatives have had colorectal cancer.
The following people are more at risk for colorectal cancer:
- Smokers.
- Heavy drinkers.
- American Indians and Alaska Natives.
- Ashkenazi Jews.
- African Americans.
- Night shift workers.
- People with Type 2 diabetes.
- Overweight or obese people.
- People who consume a lot of processed meats.
- People with a sedentary lifestyle.
- People over age 50.
- People with a family history of colorectal cancer.
- People with Lynch syndrome, the most common hereditary colorectal cancer syndrome. People with this condition should start regular colonoscopy screening by their early 20s.
- People with familial adenomatous polyposis (FAP), a syndrome characterized by hundreds of thousands of benign polyps. Due to a nearly 100 percent rate of developing colorectal cancer before age 50, individuals with this gene should start colonoscopy screening as early as 10 to 15 years old.
- People with inflammatory intestinal conditions, such as inflammatory bowel disease (IBD).
- People with Peutz-Jeghers syndrome, which involves hamartoma polyps. Screening beginning in early adolescence is recommended if diagnosed with this syndrome.
- People with MUTYH-associated polyposis, caused by a mutation resulting in many polyps. People with this genetic mutation should begin screening between 25 and 30 years old.
- People with juvenile polyposis syndrome (JPS), a rare genetic condition affecting around 1 in 100,000 people that can lead to colorectal cancer if polyp proliferation goes untreated.
What Are the Stages of Colorectal Cancer?
Colorectal cancer staging is complex but generally concerns stages 0 through 4. These stages include:
Stage 0
The cancer is in its earliest stage and has not spread past the innermost layer of the colon or rectum.
Stage 1
The cancer has grown through the mucosa and into the submucosa but has not spread to the lymph system or distant sites.
Stage 2
Stage 2 is broken into three categories:
- 2A: Cancer has grown into the outer layers of the colon and/or rectum but has not grown through these layers.
- 2B: Cancer has grown through the colon and/or rectum walls but has not spread to other tissues or the lymph system.
- 2C: Cancer has spread to nearby tissues.
Stage 3
Stage 3 is broken into three categories:
- 3A: Cancer has spread to muscular layers and nearby lymph nodes.
- 3B: Cancer has either spread through the outermost layers and to up to three lymph nodes, or it hasn’t spread past the outermost layers but has invaded four or more lymph nodes. It has not spread to distant sites.
- 3C: Cancer has spread beyond the muscular layers and into lymph nodes but has not spread to distant sites.
Stage 4
Stage 4 is broken into three categories:
- 4A: Cancer has spread to one distant organ or distant lymph nodes. It may or may not have grown through the colorectal wall and may or may not be in nearby nodes.
- 4B: Cancer has spread to more than one organ or area, which may include a distant lymph node.
- 4C: Cancer has spread to a distant area of the lining of the abdomen.
How Is Colorectal Cancer Diagnosed?
Regular testing at an earlier age for individuals genetically predisposed to colorectal cancer is a good idea. The screening tests for colorectal cancer most commonly involve a colonoscopy, but other tests can include a stool test, sigmoidoscopy, and capsule endoscopy.If you are experiencing symptoms or a screening test points toward abnormal findings, follow-up tests can be completed to confirm or rule out a diagnosis.
These tests include:
- Physical exam: Your doctor will press or palpate your abdomen for masses and may perform a digital rectal exam to feel for any abnormal areas and to check for blood in the stool.
- Blood tests: A complete blood count can help assess if you have anemia, elevated liver enzymes, or specific tumor markers like carcinoembryonic antigen (CEA).
- Colonoscopy: The entirety of the colon and rectum are examined with a small video camera attached to a fiberoptic tube.
- Proctoscopy: The inside of the rectum is examined with a small camera.
- Biopsy: A small piece of tissue is removed during a colonoscopy and analyzed for cancer cells.
- Imaging tests: Imaging tests such as X-rays, computed tomography (CT), ultrasounds, or magnetic resonance imaging (MRI) scans may be performed to help look at suspicious areas in the body or to help assess if a treatment is working.
If a diagnosis of colorectal cancer is confirmed, your doctors will stage the cancer, which helps inform which treatments can be most effective.
What Are the Complications of Colorectal Cancer?
Colorectal cancer can develop with several complications, with areas most affected being the digestive system and the nerves within this system.
Some of the most common acute complications include:
- Bleeding: Internal bleeding can be a common complication of colorectal cancer that typically presents and gets diagnosed via a blood test showing iron deficiency anemia. There can also be blood present in the stool due to colonic bleeding.
- Obstruction: A bowel obstruction can commonly occur as a complication of colorectal cancer. If someone experiences an obstruction, they may have intense abdominal pain with vomiting, fluid accumulation in the blocked bowel, and, therefore, dehydration and low electrolytes. In addition, infection may occur due to obstruction, as bacteria and toxins can build up due to not being eliminated.
- Perforation: This is a rarer colorectal cancer complication due to an obstruction. This is seen when a tumor grows, obstructs, and penetrates the intestinal wall, requiring emergency surgery.
- Jaundice: Jaundice is a yellowing of the skin that can present due to a buildup of bilirubin in the body. If cancer has spread to the liver’s biliary ducts, the metabolism of bilirubin is affected, causing jaundice.
What Are the Treatments for Colorectal Cancer?
The treatments for colorectal cancer will vary based on the advancement of the cancer, where it is located, and the person’s overall health status. Standard treatments can involve surgery, chemotherapy, radiation, immunotherapy, targeted therapies, or palliative care. The following is what some treatments entail:
- Surgery: Surgery entails removing the cancer from the colon and/or rectum. Resection of the colon may be needed in some cases to get all the cancer. If much of the colon needs removal, a person may need a colostomy bag. Following surgery, it is common to need chemotherapy or radiation to ensure all the cancer has been eradicated.
- Chemotherapy: Chemotherapy involves a cancer drug that kills cancer cells. It is injected or taken orally and may be prescribed independently or combined with other treatments.
- Radiation: Radiation uses X-rays to kill cancer cells. It is done internally via sealed portions of a radioactive substance implanted into or near the tumor as a palliative option to help reduce pain and discomfort.
- Targeted therapies: Targeted therapies refer to treatments that attack specific cancer cells and may not cause as much harm to healthier cells surrounding the cancer cells. One type of targeted therapy used for colorectal cancer is monoclonal antibodies, proteins made in laboratories that attach to cancer cells to help inhibit their growth. This treatment is usually given via IV and may accompany other treatments.
- Immunotherapy: This therapy helps boost the patient’s immune system by blocking proteins that can interfere with the body’s T cells fighting the cancer cells.
How Does Mindset Affect Colorectal Cancer?
The research is mixed regarding how optimism or a positive attitude affects cancer outcomes and perceived quality of life. While some studies indicate that keeping a positive outlook amidst a cancer diagnosis helps improve cancer patients’ quality of life, further research is needed to confirm a direct correlation.
As stated earlier, the incidence of younger-onset colorectal cancer in people under 50 is increasing. As such, the mental component of experiencing cancer at a younger age can understandably take a toll.
Research indicates that the emotional distress for younger individuals experiencing colorectal cancer is one of the most common and significant types of psychosocial impairment. In addition, the social impact and how a diagnosis affects one’s family or social relationships is also significant and plays into emotional stress. Because battling a cancer diagnosis comes with physical repercussions, individuals also noted changes sexually and in their ability to continue working, which can negatively affect their mental health status.
In addition, due to some of the possible unique consequences of colorectal cancer, like a colostomy bag, emotional distress for individuals can be higher than in other types of cancers. Especially for younger individuals, a physical bag on the outside of the body may cause embarrassment or sexual impediments, leading to increased levels of distress.
For all ages, because the cancer diagnosis is challenging to cope with, care is needed for individuals battling cancer during and long after a diagnosis or treatment. Research shows that for survivors, many concerns continue to impact individuals beyond treatment significantly.
Some of these concerns involve:
- How long cancer-related stress will continue.
- How returning to work might be.
- If their family members are at risk of developing colorectal cancer.
- How their lifestyle, activity levels, etc., may need to change.
- How their sexual life may be affected.
- Anxiety over recurrence.
While a colorectal cancer diagnosis is life-altering and has mental health ramifications, enlisting the right team of qualified health care practitioners, including doctors and therapists, is essential. Considering support groups and other ways to surround yourself with individuals who have had similar experiences can also be an empowering step.
What Are the Natural Approaches to Colorectal Cancer?
There is a shortage of randomized controlled trials examining the relationship between natural treatment approaches to colorectal cancer and successful cancer eradication. However, one 2014 study examined a Pan-Asian medicine, vitamin, and nutrition intervention and its survivorship. Specific herbal-based interventions were provided, including several Pan-Asian medicinal formulas and supplementation with nutrients like curcumin, fish oil, folic acid, coenzyme Q10, and royal jelly. While this study showed promise when combining natural approaches with chemo and other anti-cancer drugs, further studies are needed to confirm which natural treatments had the most significant effects on cancer apoptosis.
Another 2019 review examined natural nutritional approaches to fighting colorectal cancer and indicated some positive findings. For example, foods containing alkaloids, or compounds found in several plant-based foods have a tumor-suppressing effect by inhibiting growth factors that cause upregulation of cancer cells. These foods include:
- Coffee beans.
- Cacao beans.
- Tea leaves.
- Potatoes.
The study also examined compounds high in polyphenols like resveratrol (found in red grapes), curcumin (found as turmeric), and berberine, finding that the anti-inflammatory nature of these compounds can aid in cancer cell death.
Another comprehensive review indicated that other plant-based phytochemicals are shown to be helpful when fighting against colorectal cancer. The most beneficial foods with these phytochemicals included the following:
- Grapes.
- Soybeans.
- Green tea.
- Garlic.
- Olives.
- Pomegranates.
These plants are high in phytochemicals like flavonoids and polyphenols known to inhibit cancer growth. There is generally no downside to including more of these plants and herbs in the diet, so these could be a helpful addition to any colorectal treatment approach. As always, consult your doctor for more personalized information.
How Can I Prevent Colorectal Cancer?
While there is no guaranteed way to completely eradicate your chances of developing colorectal cancer, there are several steps you can take to lower the risk.
Some of the best ways to reduce your risk have to do with diet and lifestyle, including the following:
Get Screenings
If you are genetically predisposed to colorectal cancer, regular screenings are one of the best ways to take a proactive approach against cancer development. The American Cancer Society recommends beginning screenings that include colonoscopy at age 45 if you are considered at average risk.
Eat a High-Fiber Diet
Increasing your intake of fresh produce and higher-fiber foods helps to ward off colorectal cancer by optimizing the digestive system’s overall health. Increasing your fiber intake through anti-inflammatory food items like whole grains and fresh produce helps create a more optimal gut microbiome. Including several anti-inflammatory foods like omega-3 fatty fish, nuts and seeds, and olive or avocado oil is optimal.
Reducing your intake of processed meats can also help, as this aids in overall inflammation reduction. Some evidence suggests some red meat may be linked to an increased risk of colorectal cancer, but more research needs to be done to better understand any correlation. Research indicates that improving the gut microbiome and digestive regularity with high-fiber, anti-inflammatory foods can aid in reducing the risk of colorectal cancers due to less pro-inflammatory bacteria present in the gut, optimizing the overall homeostasis of the gut and colon/rectum. Consult a qualified health care practitioner like a dietitian for more personalized information.
Get Enough Vitamin D
Promising research suggests a correlation between adequate vitamin D levels and colorectal cancer prevention, especially in younger individuals. Vitamin D deficiency has been linked to increased rates of colon polyps and cancer proliferation, so avoiding a vitamin D deficiency through dietary intake and supplementation can be helpful. Including vitamin D-rich foods in the diet, such as fatty fish and dairy products, is helpful for individuals wanting to optimize cancer prevention efforts.
As always, having your vitamin D blood levels evaluated by your doctor is recommended.
Get Adequate Calcium
Research indicates that adequate calcium intake positively correlates with anti-colorectal cancer outcomes. This is thought to be because adequate calcium intake helps reduce inflammation in the colon wall and aids in reducing bile acid irritation. Including calcium-rich foods, like dairy products, tofu, and leafy greens, can be a helpful dietary addition for individuals wanting to bolster their cancer-fighting opportunities.
Exercise Regularly
Regular exercise helps to ward off colorectal cancer and promote overall well-being. If you are struggling with your weight, appropriate weight loss that may accommodate a more advantageous diet and lifestyle is also protective.
Limit Toxins
Avoiding smoking and limiting alcohol are known to be cancer-protective. For more personalized information and guidance, consult your doctor.
Medically reviewed by Beverly Timerding, MD.
Reposted from: https://www.theepochtimes.com/health/the-essential-guide-to-colorectal-cancer-symptoms-causes-treatments-and-natural-approaches-5393201
Related:
Colorectal Cancer: Study Shows Dietary Changes Can Shrink Tumors
Ivermectin for Colorectal Cancer?

.png)


.png)

.png)

Comments
Post a Comment