Acid Reflux and GERD Guide: Symptoms, Causes, Treatments, and Natural Remedies
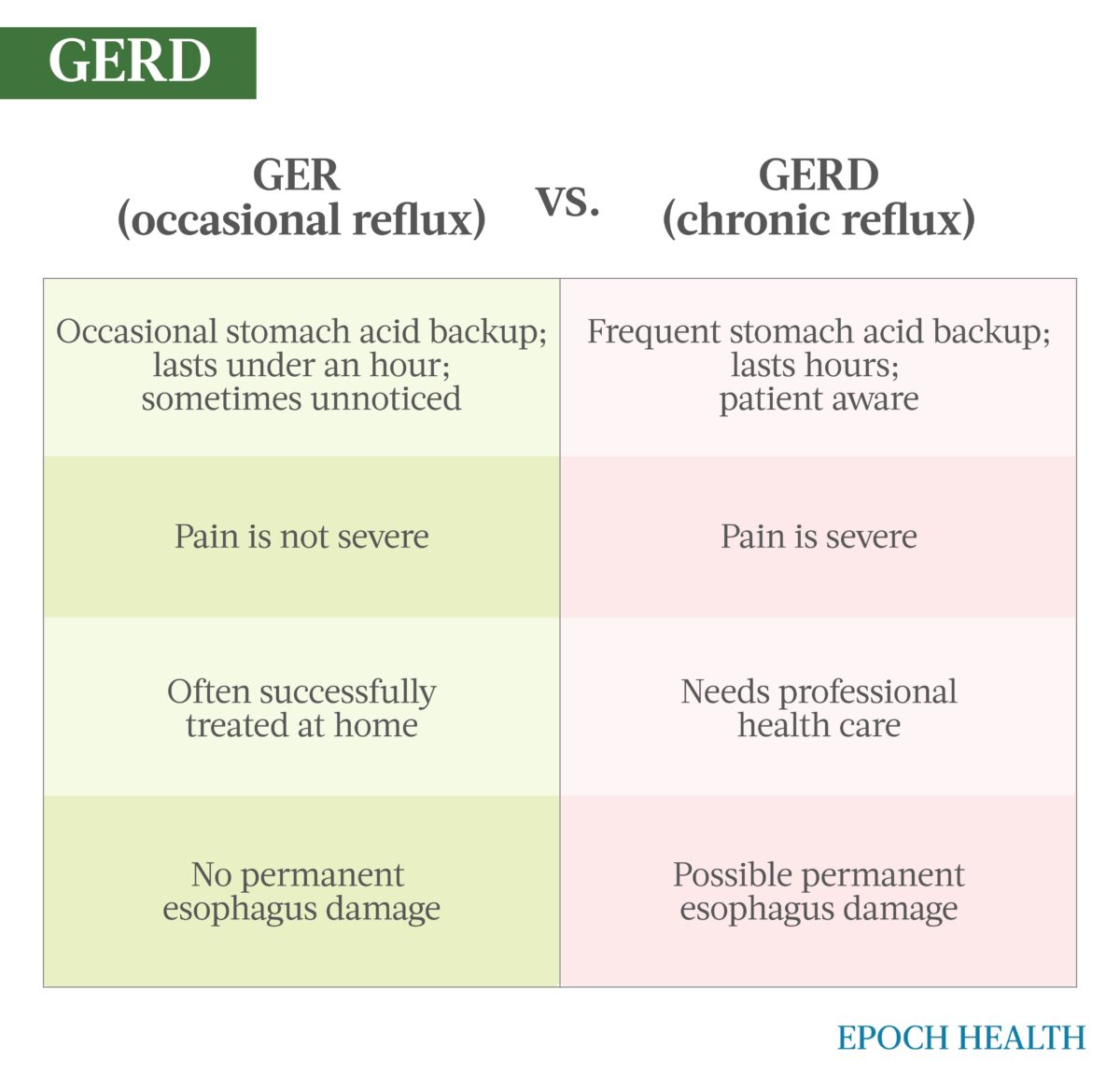
Many people experience occasional gastroesophageal reflux (GER), more commonly known as acid reflux or heartburn. According to epidemiological data from the International Foundation for Gastrointestinal Disorder (IFFGD), up to 40 percent of people experience acid reflux at least once a month, with 20 percent experiencing it on a weekly basis.
Occasional acid reflux is not a serious condition and can often be treated effectively at home. However, when acid reflux happens repeatedly and frequently, it can cause GERD—a condition in which the lining of the esophagus is damaged due to prolonged exposure to stomach acid. According to the National Institute of Health, 20 percent of Americans suffer from GERD. It can be a serious condition that should be treated in consultation with a physician.
GER Versus GERD
Most people can manage the symptoms of GERD with lifestyle changes and/or medications. In rare cases, some may need surgery to address their symptoms.
GERD Versus LPR
A lesser-known kind of acid reflux is laryngopharyngeal reflux (LPR)—sometimes called “silent reflux.” This is caused by the same dysfunction of the LES, but in LPR, stomach acid backs up all the way to the larynx (voice box) or the pharynx (back of the throat). It is called silent reflux because it is harder to diagnose in adults, though the condition is common in infants whose sphincter muscles have not yet fully developed. Only one or two of the symptoms listed below may be present in the case of LPR.
GERD Symptoms
Symptoms occur twice a week or more and may include:
- Difficulty swallowing.
- Burning sensation in the chest.
- Chest pain when lying horizontally.
- Burning sensation in the throat.
- Bad taste in the back of the throat.
- Reflux that occurs at night and wakes you.
LPR Symptoms
Symptoms may be chronic or rare and may include:
- Difficulty swallowing.
- Chronic cough.
- Hoarseness.
- Sore throat.
- Postnasal drip or mucus in the back of the throat.
- Red, swollen, or sore voice box.
- The feeling of a lump in the throat that doesn’t go away.
- Difficulty breathing.
LPR is a serious condition that can result in a scarred throat and voice box. It can also increase risk for cancer in these areas, impact the lungs, and aggravate conditions such as asthma, emphysema, or bronchitis. If you think you have either GERD or LPR, consult a physician as soon as possible.
What Are the Symptoms and Early Signs of GERD?
As described by the IFFGD, “the two most frequently reported symptoms of GERD are heartburn, which can be described as a burning discomfort that begins behind the breastbone and radiates to the neck and throat, and acid regurgitation, which is characterized as a bitter, sour tasting fluid.”
Sometimes patients suffer from other symptoms, such as:
- Cough
- Laryngitis
- Asthma
- Difficulty swallowing
- Hoarseness in the morning
The condition can also cause bad breath. Some GERD patients have no apparent symptoms.
What Causes GERD?
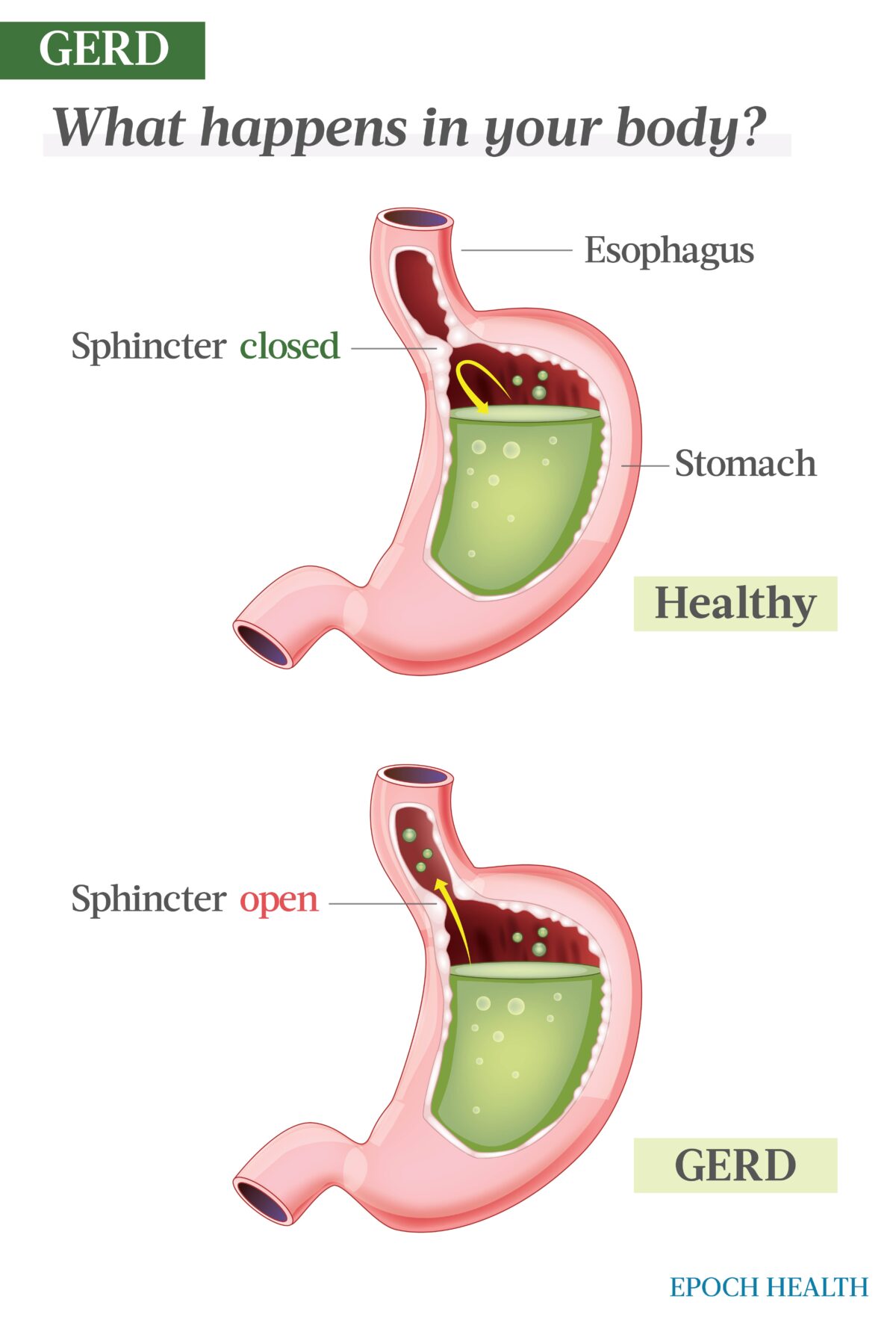
Acid reflux is caused by the failure of the sphincter muscle connecting the esophagus to the stomach to properly close after opening to admit food and drink.
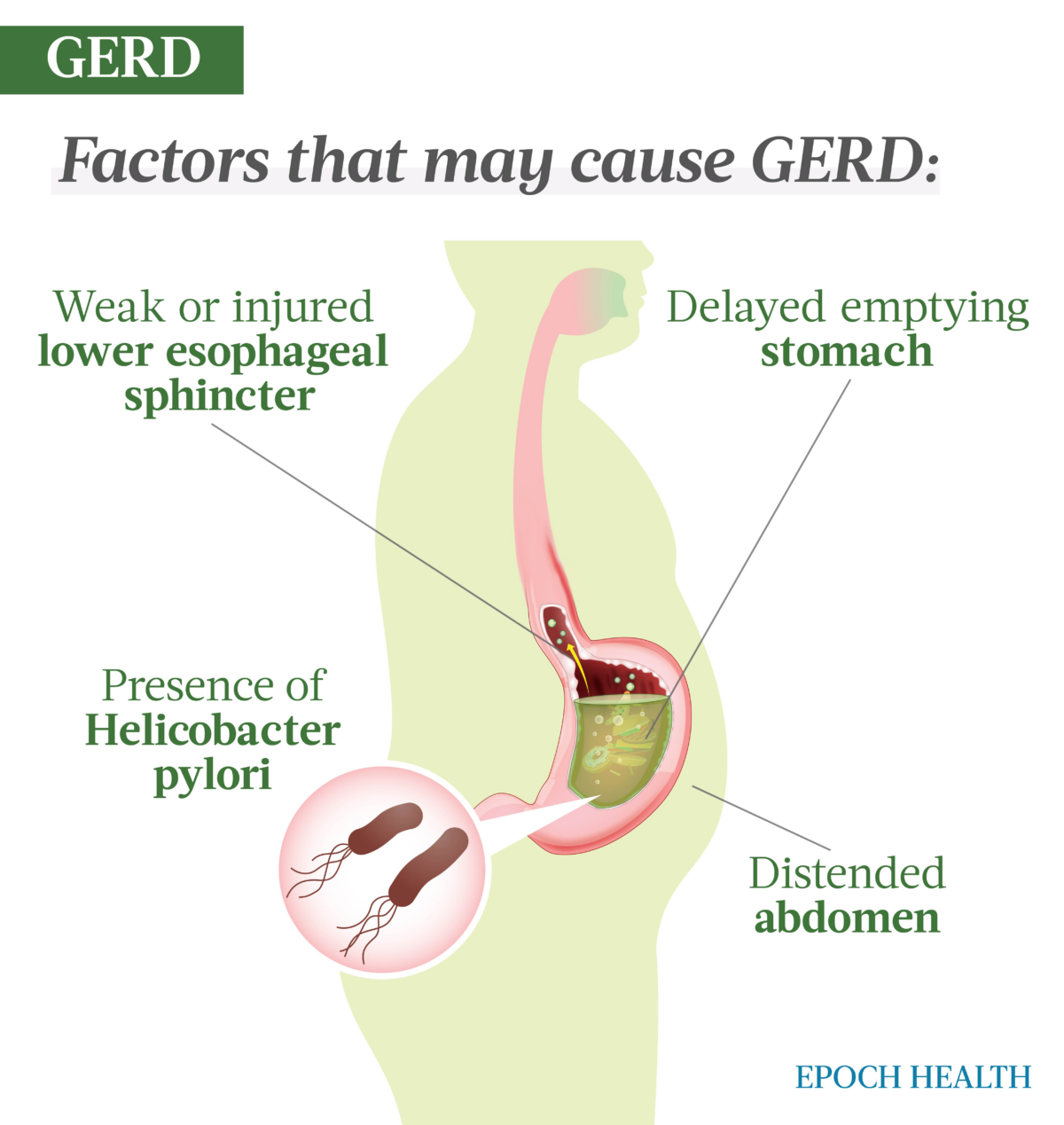
Researchers have not isolated a single cause for this problem. Certain physical factors may cause GERD, including:
- Weak or injured LES.
- Abdominal distention (as accompanies pregnancy or obesity).
- Delayed emptying of stomach content.
- Presence of the bacteria Helicobacter pylori.
Who Is More Likely to Develop GERD?
Research indicates that many factors can contribute to the development of the disease. Some are non-modifiable factors such as gender, age, or genetic factors. Among contributing modifiable factors are lifestyle, diet, and excessive body weight. Lifestyle risk factors include:
- Excess body weight, particularly obesity.
- Moderate to high alcohol use.
- Smoking.
- Exercising immediately after a meal.
- Lack of regular exercise.
- Diet and eating habits.
In terms of diet, a number of foods likely to trigger acid reflux have been identified, including:
- Fried and fatty foods.
- Sour and spicy dishes.
- Acidic foods such as citrus fruits and tomatoes.
- Carbonated beverages.
- Black tea.
- Coffee (including decaf).
- Chocolate.
- Alcohol.
Eating habits such as irregular mealtimes, overeating, and eating meals just before bedtime have also been correlated with the symptoms of GERD.
What Are the Tests to Detect GERD?
Your physician is likely to make an initial diagnosis based on your symptoms and eating habits. However, positive confirmation, including the ruling out of other conditions such as heart disease, requires testing.
To confirm a diagnosis, your physician may order one or more of the following:
- Upper endoscopy: This is a procedure in which a tube with a light and a camera is inserted down the throat, allowing your physician to see inside your esophagus and stomach. This is sometimes done simultaneously with a colonoscopy, though the procedures can be done separately. While this procedure will not always give a positive confirmation of the initial diagnosis, it will show whether any damage to the digestive system has occurred due to GERD.
- Transnasal esophagoscopy: This test looks for esophagus damage. A thin, flexible tube with a video camera is inserted through the nose, down your throat, and into the esophagus. The camera then sends photos to a video screen. This procedure requires no anesthesia and can be done in your doctor’s office.
- X-ray of the upper digestive system: X-rays are taken after you drink a chalky prep liquid that coats the lining of the digestive tract. The coating gives your doctor a clear silhouette of your esophagus and stomach. This is particularly helpful in evaluating people who are having trouble swallowing. This procedure may also involve swallowing a barium pill that can help diagnose a narrowing of the esophagus.
- Esophageal manometry: This measures the rhythmic muscle contractions in the esophagus upon swallowing. Esophageal manometry also assesses the coordination and force of the working muscles of the esophagus. This test is typically only recommended for people who have difficulty swallowing.
- Ambulatory acid (pH) probe test: This test is the “gold standard” for testing for GERD. A clip or small tube is placed in your esophagus to assess how often and how much stomach acid regurgitates. The monitor connects to a small computer that you wear over your shoulder or at belt level.
The wide range of symptoms for GERD contributes significantly to the expense of tests needed to rule out other conditions. For example, the expense of excluding heart attacks and other cardiac problems can be quite costly.
What Are the Complications of GERD?
According to the American Gastroenterological Association, untreated GERD can lead to:
- Esophagitis: inflammation of the esophagus
- Stricture: The esophagus narrows due to ulceration and scarring, making it hard to swallow and causing food to become lodged in the esophagus.
- Breathing problems: asthma or chronic cough, etc.
- Barrett’s esophagus: a change in the tissue lining your esophagus that elevates your risk for esophageal cancer
GERD can also lead to complications beyond the esophagus, including inflammation of the pharynx and larynx. It may also affect the lungs, causing bronchitis, asthma, or pneumonia.
What Are the Treatments for GERD?
GERD is treated with diet and lifestyle adjustments, medication, and, in rare instances, surgical intervention.
Diet and Lifestyle
Diet and lifestyle are crucial first steps in treating GERD. Recommendations to relieve symptoms include:
- Achieving and maintaining a healthy weight.
- Stopping smoking, if you smoke.
- Eating frequent, smaller meals rather than fewer, large ones.
- Decreasing the amount of fat in your diet, including fatty meats, gravy, butter, oils, salad dressings, and full-fat dairy products (e.g., whole milk, cheese, and sour cream).
- Sitting upright while eating and remaining upright (standing or sitting) for an hour afterward. (No slouching on the couch after a meal.)
- Not eating for at least three hours before going to bed.
- Avoiding clothes that are tight in the belly area. By squeezing the stomach, they can push acid upward into the esophagus.
- Sleeping with the head of your bed raised 6 to 8 inches. You can elevate the bed by putting blocks under the bedposts. (Note: Extra pillows won’t work as this will squeeze the stomach.)
- Cutting out possible trigger foods, including spicy or sour foods, and liquids such as coffee, alcohol, and vinegar-based products that can affect the muscular movements of the digestive tract.
Medications
If your condition doesn’t respond to these lifestyle and diet changes, your doctor may prescribe medication. For GERD, these medications are either designed to decrease your levels of stomach acid or increase the peristalsis (muscular movement) of the upper digestive tract, forcing the acid back down into the stomach where it belongs.
- Antacids: Over-the-counter antacids are best for relatively infrequent discomfort due to reflux. Antacids can worsen the problem if taken too often, as they can cause the stomach to produce more acid.
- Histamine blockers: Histamine 2 (H2) blockers are designed to lower acid secretion. H2 blockers help heal esophageal damage in about half of the patients who take them.
- Proton pump inhibitors: Proton pump inhibitors (PPIs) block the three primary acid production pathways. PPIs suppress acid production significantly more than H2 blockers. Many patients, even those with severe damage to the esophagus, have experienced healing of esophageal damage when prescribed PPIs. Baseball Hall of Famer and sportscaster Jim Palmer has promoted their efficacy in treating his decades-long battle with GERD.
- Prokinetic agents: Prokinetic agents are drugs that enhance the smooth muscle activity of your gastrointestinal tract. Your doctor may prescribe them in combination with an acid-suppressing drug.
Surgery and Endoscopic Intervention
- Nissen fundoplication: A surgical intervention may be recommended by your doctor if your treatment does not respond to lifestyle and medication changes. The goal of such surgery is to reinforce the anti-reflux barrier. In the procedure, the surgeon wraps a part of the upper stomach around the lower esophagus, enhancing the action of the LES. The procedure may also be done laparoscopically to reduce recovery time. Some patients choose this option over a lifetime of taking medication.
- Transoral incisionless fundoplication (TIF): A TIF is an alternative to surgery for some. It uses a device to create a passageway for an endoscope. In the procedure, the physician deploys preloaded tweezers and fasteners in the device to repair or reconstruct the lower esophageal sphincter. One form of therapy uses an endoscopic “sewing machine” to install stomach sutures that increase the anti-reflux barrier.
- LINX device: Using minimally invasive surgery, a surgeon wraps a ring of magnetic beads around the LES. The magnetic attraction between the beads keeps the LES closed to refluxing acid but allows food to pass. The magnetic beads do not interfere with airport security systems or magnetic resonance imaging.
How Does Mindset Affect GERD?
Research has shown a link between GERD and psychological factors. In a seminal 2016 study of over 1,200 firefighters, researchers found a higher incidence of depression, stress, and low self-esteem among GERD sufferers than among those firefighters who were GERD-negative. The researchers concluded, “psychological and medical approaches should be combined in GERD assessment.”
Some research has shown a connection between anxiety and GERD. If this is true in your case, you may want to speak with your doctor about medications to treat anxiety and/or depression. Activities that reduce anxiety such as meditation, yoga, “forest bathing,” regular exercise, or breathing exercises may also help address your symptoms.
The Importance of Sleep
Researchers have also found an association between GERD and poor sleep quality.
The exact relationship is not understood, but researchers have suggested that improved sleep could also alleviate the symptoms of GERD.
Discuss your sleep habits with your physician or health care provider. They may recommend supplementing melatonin or changes like using blackout blinds, white noise machines, removing or disabling electronics in your sleep space, and more.
What Are the Natural Remedies for GERD?
At least two studies have had promising results treating GERD symptoms with extracts obtained from Opuntia ficus-indica, commonly known as prickly pear cactus.
According to Harvard Medical School, licorice, chamomile, and marshmallow root have been found to be effective in treating GERD in several studies. Slippery elm and d-limonene also have anecdotal evidence supporting their use.
How Can I Prevent GERD?
While nothing you can do will be 100 percent effective in preventing GERD, losing weight if you are overweight and stopping smoking if you smoke are two lifestyle choices that can make a big difference. Reducing or stopping the usage of certain medications that can aggravate acid reflux/GERD may also be effective, though you should consult your physician before discontinuing or lessening your medications. Medications that aggravate GERD are:
- Benzodiazepines, a class of sedatives.
- Calcium channel blockers to treat high blood pressure.
- Certain asthma medications.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Tricyclic antidepressants.
As indicated above, eating and sleeping well in addition to lifestyle choices to manage stress and anxiety can also help control acid reflux/GERD.
Medical reviewed by Beverly Timerding, M.D.
Gaviscon Extra Strength Cherry Chewable Tablet For Fast-Acting Heartburn Relief (Amazon's Choice)
About this item
- Gaviscon provides fast acting, long lasting heartburn relief and is an acid reflux remedy (when used as directed)
- Relieves heartburn, sour stomach, acid indigestion, and upset stomach associated with these symptoms
- Quickly neutralizes stomach acid and helps keep acid down for hours (when used as directed)
- Gaviscon is gastroenterologist recommended for heartburn and is available in both liquids and chewable tablets
- Gaviscon Extra Strength Tablet Antacid Cherry flavor contains the active ingredients aluminum hydroxide and magnesium carbonate
- HSA and FSA eligible product




.png)




Comments
Post a Comment