Chronic Fatigue Syndrome: Symptoms, Causes, Treatments and Natural Remedies 2023
Chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis (ME), is a disabling and complex disorder, and according to the U.S. Centers for Control and Prevention (CDC), is estimated to affect up to 2.5 million Americans. Up to 90 percent of sufferers are undiagnosed. The CDC estimates the disease costs the U.S. economy about $17 to $24 billion annually in medical bills and lost income.
The condition causes extreme physical and mental fatigue that lasts for at least six months and more often affects women than men. Symptoms worsen with physical or mental activity and, unlike normal experiences of fatigue, don’t substantially improve with rest.
Because of the lack of a clear understanding of the disease, its causes, prevention, and treatment are all subjects of medical research and debate.
What Are the Symptoms and Early Signs of Chronic Fatigue Syndrome?
People with CFS have overwhelming fatigue that is not improved by rest. Sufferers cannot do their usual activities or do them at the same level as before they were affected. At times, CFS may confine them to bed.
CFS tends to worsen with physical or mental activity. Doctors call this postexertional malaise (PEM). Other CFS symptoms include problems with sleep (insomnia or unrefreshing sleep), thinking and concentrating (“brain fog”), nonspecific physical pain, and vertigo/dizziness.
People with CFS may not look ill. However, they:
- Are unable to function as they did before becoming ill.
- Suffer from an impaired ability to accomplish daily tasks, like washing the dishes or cooking a meal.
- Often struggle with keeping a job, attending school, and participating in family and social life.
CFS can become chronic and seriously disabling. According to the CDC, at least 1 in 4 patients is bed- or house-bound for long periods during their illness.
Other symptoms can include:
- Problems sleeping, such as insomnia.
- Muscle and/or joint pain.
- Headaches.
- Sore throat or sore glands without swelling.
- Aggravation of symptoms with mental or physical exertion.
- Problems with concentration, short-term memory, and trouble speaking or understanding speech.
- Flu-like symptoms.
- Dizziness or nausea.
- Accelerated or irregular heartbeats.
What Causes Chronic Fatigue Syndrome?
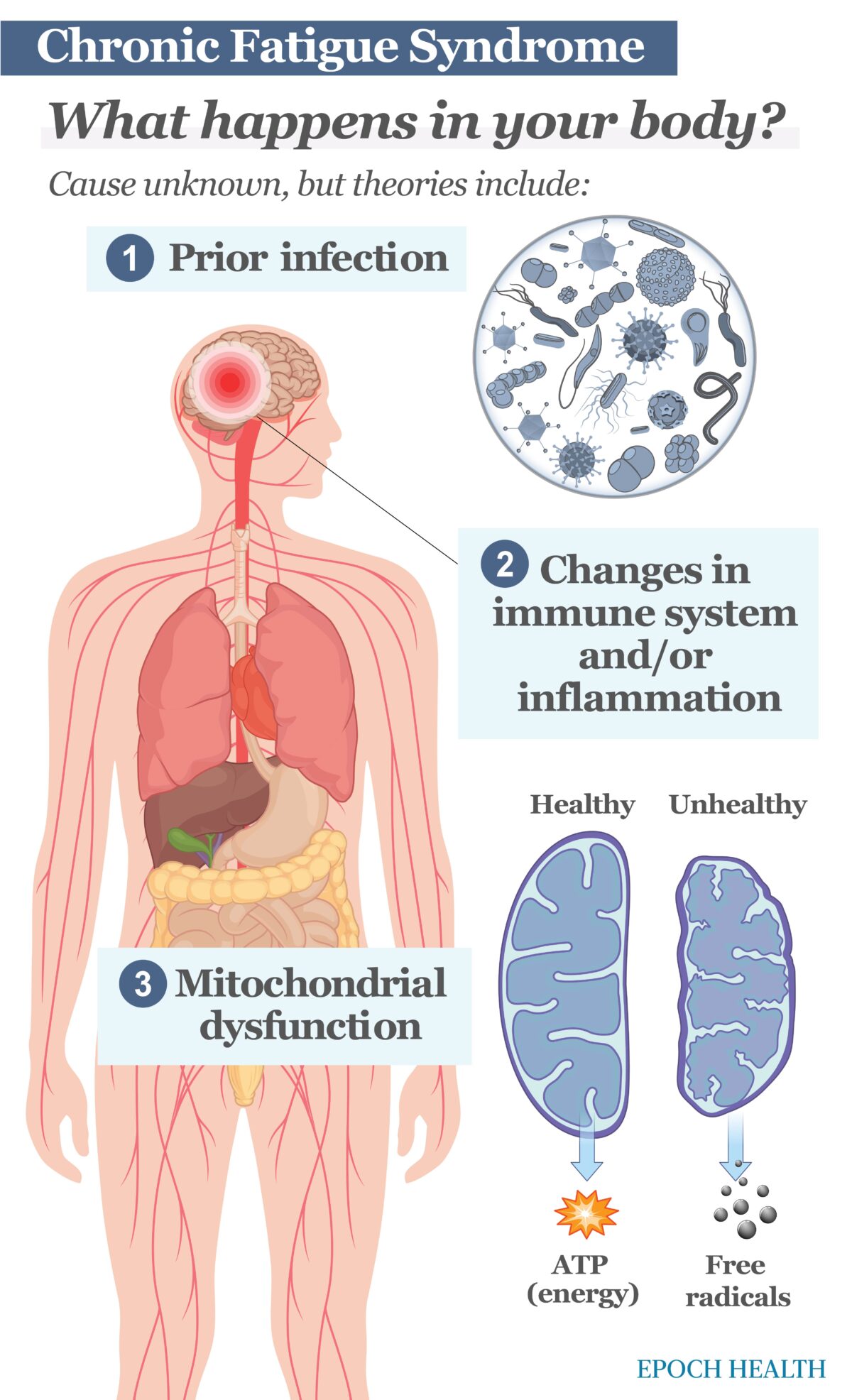
Researchers have not yet found what causes CFS, but there are several possibilities. Some factors may include genetics, trauma, or issues with energy use; however, the main theories include prior infection, autoimmune changes, stress, and mitochondrial dysfunction.
Prior Infection
For some, the onset of CFS is reminiscent of coming down with the flu. This flu is often particularly severe and of unusual duration—dubbed by at least one expert as the “drop-dead flu.” Consequently, the initial diagnosis for CFS is often “postviral fatigue (PVF),” frequently changed to chronic fatigue syndrome when the symptoms remain unimproved after six months.
This has made some researchers suspect that an infection triggers CFS. Close to 1 in 10 individuals infected with Epstein-Barr virus, Ross River virus, or Coxiella burnetti will develop symptoms that meet the criteria for CFS. People who have had severe symptoms with these infections are more likely than those who had mild symptoms to later develop CFS. But not all people with CFS have had these infections, so prior infection is not a definitive indicator.
Other infections that have been studied in connection with CFS are:
- Human herpesvirus 6
- Enteroviruses
- Rubella
- Candida albicans
- Bornaviruses
- Mycoplasma
- Human immunodeficiency virus (HIV)
However, according to the CDC, no direct link between these infections and CFS has been discovered.
The descriptions of long COVID also match closely those of PVF and CFS, such that some top experts on CFS have suggested that long COVID is indistinguishable from it.
Changes in the Immune System
CFS may be caused by a change in the person’s immune system and the way it responds to infection or stress. CFS shares some features of autoimmune illnesses (diseases in which the immune system attacks healthy tissues in one’s own body, such as rheumatoid arthritis). For example, both CFS and most autoimmune diseases are more common in women, and both are characterized by increased inflammation. However, other signs of autoimmune disease, like tissue damage, have not been found in patients with CFS.
Mitochondrial Dysfunction
A recent study in the UK found that the cells of CFS patients were less able to produce additional energy in response to stress. Specifically, the mitochondria within these cells were less able to increase energy production, only increasing energy production by up to 44 percent. This contrasted with normal cells that increased energy production up to 98 percent in response to stress. The normal cells were able to consume twice as much oxygen in response to stress as compared to the cells of CFS patients.
Stress and the HPA Axis
Some doctors see CFS as a dysfunction of the hypothalamic-pituitary-adrenal axis (HPA axis). The HPA axis is a complex network that controls the body’s reaction to stress and regulates a host of processes such as the immune response, digestion, energy usage, and mood. Physical or emotional stress can affect this axis.
HPA axis regulation involves connections between three parts of the nervous system: the hypothalamus, the pituitary glands, and the adrenal glands. These release hormones, like corticotrophin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), cortisol, and others. When these hormones become imbalanced, many body systems and functions, including the immune response, can be affected.
Cortisol, also known as the “stress hormone,” helps lower inflammation and calms the immune response. Although too high of a level of cortisol has been associated with anxiety, weight gain, high blood pressure, and Cushing syndrome, low levels of cortisol can be just as debilitating. Low levels of cortisol increase inflammation and put the immune system into a state of chronic activation.
Individuals with CFS commonly report physical or emotional stress before they become ill. Some CFS patients have cortisol levels lower than healthy people, but still within the normal range. Some doctors prescribe cortisol for CFS patients with lower-than-normal levels.
There are several ways you can naturally increase cortisol, including cultivating a regular sleeping pattern, eating grapefruit, taking supplements like licorice—not the candy but a dietary supplement—iron, and Panax ginseng. Avoiding refined flours and sugars, as well as eating foods rich in iron, can also boost cortisol levels.
If you see an endocrinologist who specializes in treating CFS, blood tests may be taken to determine your hormone levels. If indicated, you may be prescribed various hormone treatments to try to rectify the imbalances in your HPA axis. Some patients have experienced significant relief from symptoms with these treatments.
Who Is More Likely to Get Chronic Fatigue Syndrome?
Risk factors for chronic fatigue syndrome include:
- Age: CFS can develop at any point in life, but most commonly affects people between the ages of 21 and 60.
- Gender: Women are diagnosed with CFS four times more often than men, possibly because women are more likely to discuss their symptoms with a doctor.
- Other medical problems: People with a history of other complex medical problems, such as fibromyalgia or postural orthostatic tachycardia syndrome, may be more likely to develop CFS.
- Stress: Chronically stressed patients are more likely to overtax their hormonal system and HPA axis, which can lead to a cascade failure, causing CFS.
What Are the Tests to Detect Chronic Fatigue Syndrome?
There’s no specific test for CFS, but evaluation begins by reviewing your medical history with your doctor and having a physical examination. Lab work such as blood and urine tests will rule out other conditions, such as anemia (lack of red blood cells), an underactive thyroid gland, or liver and kidney problems. A diagnosis of CFS takes time since all other possible diseases must be excluded first.
Guidelines proposed by the United States Institute of Medicine define the fatigue characteristic of CFS as:
- Interfering considerably with the ability to engage in pre-illness activities.
- Persisting for more than six months, but has not been lifelong in duration.
- Not substantially alleviated by rest.
- Worsened by physical, mental, or emotional exertion.
To meet the Institute of Medicine’s CFS diagnostic criteria, a person would also need to suffer at least one of these two symptoms:
- Difficulties with focus, memory, and concentration
- Lightheadedness that worsens when standing from a sitting or lying down position
The guidelines also note that these symptoms must continue for at least six months and be present “at least half the time with moderate, substantial, or severe intensity.”
Typically, patients also experience some of the symptoms mentioned earlier in the Symptoms section.
Will CFS Increase the Risk of Other Diseases?
Some overlapping conditions with CFS have been identified, such as tinnitus, irritable bowel syndrome (IBS), and depression, but no causal connections have been established. The research shows distinct differences between depression associated with CFS and a typical diagnosis of clinical depression. Some research has linked CFS with somewhat elevated rates of certain kinds of cancer, notably non-Hodgkin lymphoma. The disease has also been associated with above-normal rates of suicide. Further research, however, needs to be done to confirm either of these correlations.
In general, the complications of CFS are personal, financial, and behavioral as many sufferers are simply unable to live, work, and socialize as they did before contracting the illness.
What Are the Treatments for Chronic Fatigue Syndrome?
Even though there is no cure or one single way of managing CFS that works for everyone, there are several treatment options.
Your doctor can discuss all treatment options with you, explaining the benefits and risks of each treatment. It will be necessary to develop a treatment plan adapted to your level of fatigue and circumstances.
You may need advice about making lifestyle changes and specialized treatments. There are several specialized treatments for CFS.
Cognitive Behavioral Therapy (CBT)
If you have mild or moderate CFS, you may respond to cognitive behavioral therapy (CBT). CBT is a talking treatment that can help you manage your symptoms by changing your thinking and behavioral patterns. Choose a CBT therapist who has experience dealing with CFS and treatment can offer treatment on a one-on-one basis.
Using CBT does not mean CFS is considered a psychological condition. CBT is used to help people manage a variety of long-term conditions.
Energy Management
Energy management aims to teach you how to make the best use of your energy levels in your day-to-day life, without making symptoms worse. As part of the treatment, you may be advised to monitor daily activities using a journal or phone app.
Some people with CFS have found that exercise programs can alleviate symptoms. But for some, exercise made no difference or even worsened symptoms. If you think exercise can help you, discuss a personalized plan with a health professional (such as a physical therapist) with experience working with people with CFS. In general, sufferers should increase physical activity as much as possible without aggravating symptoms.
Medication
There’s no specific medicine for treating CFS, but some drugs may be used to relieve some symptoms.
Over-the-counter painkillers can be used to treat headaches, as well as muscle and joint pain, associated with CFS. Your physician may prescribe stronger painkillers, typically only on a short-term basis.
Antidepressants are sometimes prescribed for people with CFS who are in pain or having trouble sleeping, or to deal with the depression that can result as one faces the condition. Amitriptyline is a low-dose tricyclic antidepressant sometimes prescribed to help ease muscle pain.
Some doctors have also found that intermittent use of zolpidem helps CFS patients achieve deeper, long-lasting sleep, which is often elusive for CFS sufferers. The effect is rapid, and for safety, one should be in bed within minutes of taking it. Regular long-term use results in tolerance.
How Does Mindset Affect Chronic Fatigue Syndrome?
In the 2010 American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society’s (AMECFSS) survey of treatment modalities, nearly 50 percent (pdf) of CFS patients indicated that meditation and relaxation techniques were helpful. Those who meditate regularly report an increased feeling of calm and an improved outlook on life. Meditation is also effective in controlling the pain generated by an overreactive nervous system. Like rest, meditation seems to cause no damage and results only in a general sense of improvement.
Patients with CFS, especially those who find themselves plagued by depression, anxiety, fear, and anger, can benefit greatly from the practice and philosophy of “letting go.”
What Are the Natural Remedies for Chronic Fatigue Syndrome?
Diet and Supplements
Research on the connection between diet and CFS remains relatively scant and inconclusive, but some approaches may help.
Research has yet to establish a specific diet effective in treating CFS. However, the AMECFSS recognizes the value of a healthy diet in managing CFS symptoms, including eliminating foods that seem to exacerbate symptoms.
A 2018 review on nutritional treatments for CFS published in Biomedicine and Pharmacotherapy found that many people with CFS have vitamin, mineral, and essential fatty acid deficiencies. According to the analysis, vitamin A and vitamin E are specifically promising vitamins that need further examination.
A 2017 review of studies on diet and supplements published in the Journal of Nutrition and Human Dietetics found evidence that some supplements improved fatigue and other symptoms. These included:
- Probiotics
- Coenzyme Q10
- Polyphenols (especially from dark chocolate)
- Nicotinamide adenine dinucleotide hydride (NADH)
In addition to these, other doctors have recommended:
- Megadoses of vitamin C (1,000 to 3,000 mg/day)
- Intravenous B-12
- Magnesium supplements
- B-complex supplements
One study found that the specific polyphenols in dark chocolate minimized symptoms associated with CFS. These polyphenols are also contained in foods like green tea, berries, and legumes, but they haven’t been individually studied.
Polyphenols and other types of antioxidants are believed to reverse free radical damage that may cause illness. One theory about the underlying mechanisms of CFS is that oxidative stress has a role, and these antioxidants combat the free radicals that cause this kind of stress.
A review of 22 studies also suggested that supplementing with either D-ribose or omega-3 fatty acids may reduce some symptoms of CFS.
These studies focused mostly on supplementing diet because low nutrient levels were discovered in people with CFS. Eating foods rich in these nutrients may also help alleviate symptoms, with or without supplements.
How Can I Prevent Chronic Fatigue Syndrome?
Since the causes of CFS are not established, there is no clear prevention protocol for the disease. Chronic stress can make one more vulnerable to an infection that might precipitate CFS as well as lead to a dysfunction of the HPA axis. Thus, managing stress, sleeping and eating well, and practicing good habits of mental health can all reasonably be expected to help reduce the odds of contracting CFS.
Sleep, Rest, and Relaxation
Some studies have explored a potential connection between CFS and sleep deprivation. Some evidence suggests that people with CFS get less sleep and have less rapid eye movement (REM) sleep than people without the condition. This is an area of ongoing research.
You may have sleep problems that make your CFS symptoms worse, such as:
- Problems getting to sleep.
- Unrefreshing or restless sleep.
- An excessive amount of sleep.
- Sleep during the day and insomnia at night.
CFS patients need to establish a normal sleeping pattern. Too much sleep does not usually improve symptoms and sleeping during the day can cause insomnia at night. Work with your doctor to establish a functional sleep program.
The Sleep Foundation offers a useful guide to improving your quality of sleep through behavioral, environmental, and dietary changes. If sleep does not improve with these alterations, there may be an underlying sleep problem to address.
If you need to rest during the day, your doctor should help you determine the best way to do this. For example, he or she may suggest limiting rest periods to half an hour and suggest relaxation techniques, such as breathing exercises.
Many CFS sufferers also experience light and noise sensitivity. Many patients have found that working under fluorescent lights, for instance, exacerbates both physical and mental fatigue. Changing the lighting of your home and workspace from fluorescent to LED and incandescent lighting can help improve your energy levels.
CFS is a recognized disability under the Americans with Disabilities Act (ADA), so you may be able to work with your employer to get reasonable accommodations for your workspace.
Too much bed rest can cause complications, including pressure sores and blood clots. These problems, and how to avoid them, should be discussed with your doctor and caregivers.
Exercise
Too much exercise can lead to post-exertional malaise (PEM) in which sufferers have less energy after exercise and may not recover their previous strength for days (or longer). The issue of exercise is highly controversial in the field of CFS. Some research has suggested that a program of graded exercise therapy (GET) can benefit patients, but an entire issue of the Journal of Health Psychology was devoted to calling this approach into question. The question of whether exercise is good for patients—and if so, how much—is still an unanswered question, as evidenced by ongoing research at the Mayo Clinic.
Though there are subtle differences in their approaches, both the CDC and the ME Association of the UK advise that exercise should be paced and gradual—and typically under the guidance of a trained professional.
Chronic Fatigue Syndrome vs fibromyalgia
Chronic pain and fatigue are common symptoms of both fibromyalgia and chronic fatigue syndrome. The difference is that, in fibromyalgia, fatigue often takes a backseat to debilitating muscle pain. In chronic fatigue syndrome, people have an overwhelming lack of energy, but also can experience some pain.Helpful Resources
This is a very helpful resource, particularly to help you prepare for a doctor’s visit to discuss your symptoms. CFS diagnosis often takes a year or more from onset to be confirmed. This toolkit can help lessen the time from onset to confirmed diagnosis.
“From Fatigued to Fantastic!” 4th Edition, Dr. Jacob Teitelbaum
This is a bestselling book on CFS and is widely regarded by other doctors as the best text available for laymen. Dr. Teitelbaum has been researching and treating CFS in a clinical setting for over 30 years. His newest edition covers all the modalities of treatment mentioned above, as well as a section on the “mind/body/spirit connection (MBS).”
Though this is a UK organization, it provides useful resources for dealing with CFS, postviral fatigue, and long COVID. The organization has been in operation since 1980; in some ways, treatment and research of CFS are further along in the UK than in the United States since the disease has been historically treated with less skepticism there.American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society
The counterpart to the UK ME Association, the AMECFSS has a website that offers support, access to doctors specializing in treating CFS, information on the latest research, and more.
What to Eat When You Have Chronic Fatigue Syndrome
An excellent overview of the state of the research on diet, nutrition, and CFS with practical dietary and supplement advice.
About the Author: David Charbonneau, Ph.D., is a freelance journalist who has also taught literature and writing at the college level for 25 years. In addition to The Epoch Times, his work has appeared in The Defender, Medium, and other online and print platforms. A staunch advocate for medical freedom, he lives and works in Pasadena, California.
Adapted from: https://www.theepochtimes.com/health/the-essential-guide-to-chronic-fatigue-syndrome-symptoms-causes-treatments-and-other-remedies_5163867.html






.png)

Comments
Post a Comment