Pericarditis vs Myocarditis vs Endocarditis: What's the Difference?
Introduction
Pericarditis, myocarditis, and endocarditis are all conditions that affect the heart, but they are distinct and have different causes, symptoms, and treatments. We will discuss these three conditions and highlight their differences, similarities, causes, symptoms, diagnosis, and treatment.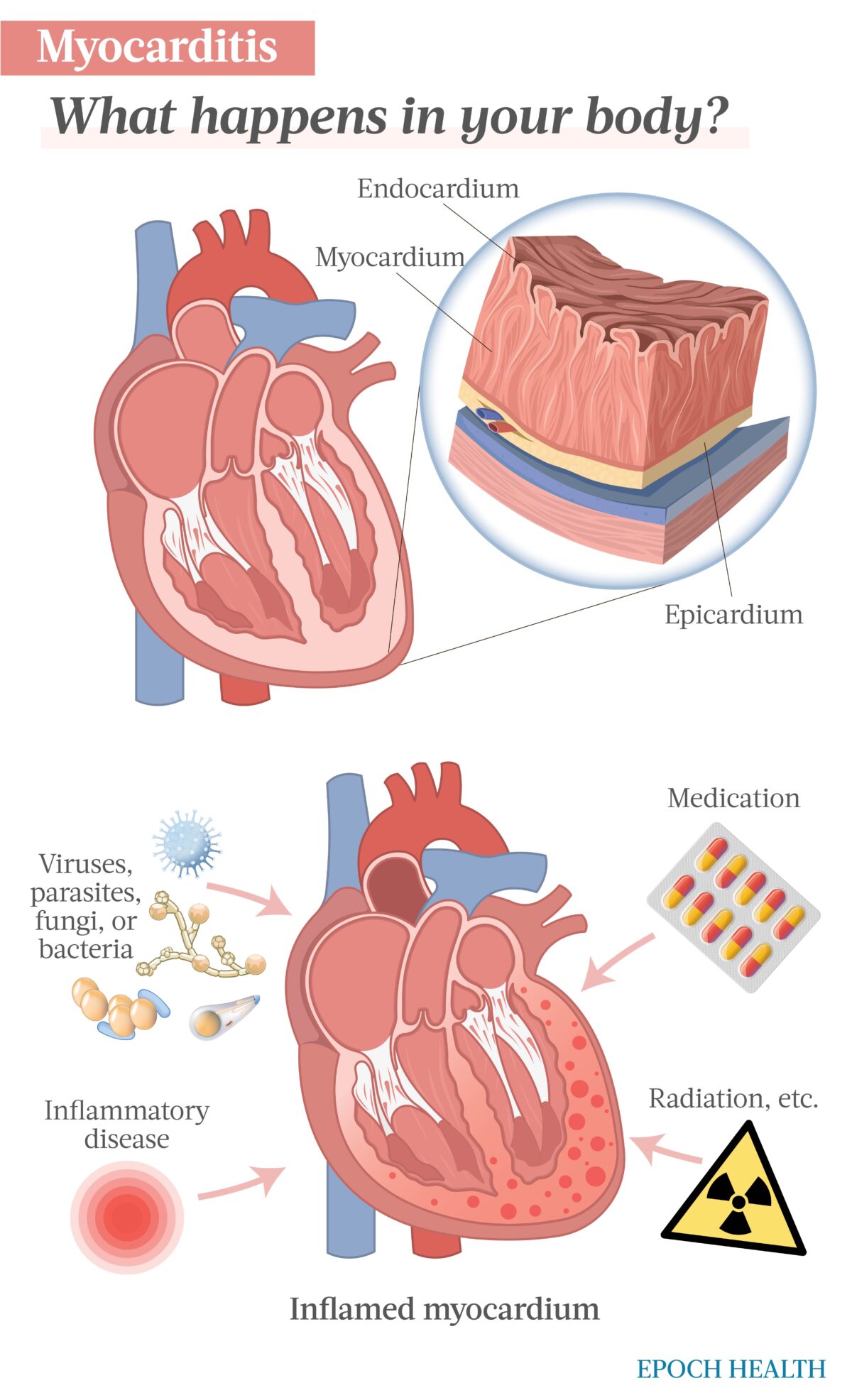
Pericarditis
Pericarditis is the inflammation of the pericardium, the thin sac that surrounds the heart. The pericardium has two layers: the outer fibrous layer and the inner serous layer. When the serous layer becomes inflamed, it rubs against the outer layer, causing chest pain and other symptoms. Pericarditis can be acute or chronic, and it can be caused by viral, bacterial, fungal, or parasitic infections, autoimmune disorders, cancer, trauma, or drugs.The symptoms of pericarditis include sharp, stabbing chest pain that worsens with deep breathing or coughing, fever, fatigue, shortness of breath, cough, abdominal or leg swelling, and palpitations. The diagnosis of pericarditis is based on the patient's medical history, physical examination, electrocardiogram (ECG), echocardiogram, blood tests, and imaging studies such as chest X-ray or MRI.
The treatment of pericarditis depends on the underlying cause and severity of symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen are commonly used to relieve pain and inflammation. Colchicine, a medication used to treat gout, can also reduce the recurrence of pericarditis. In severe cases, corticosteroids or immunosuppressive drugs may be prescribed. Pericardiocentesis, a procedure in which a needle is inserted into the pericardial sac to remove excess fluid, may be needed if there is a large effusion or tamponade.
Myocarditis
Myocarditis is the inflammation of the myocardium, the muscle layer of the heart. Myocarditis can be caused by viral, bacterial, fungal, or parasitic infections, autoimmune disorders, drugs, toxins, or idiopathic factors. Myocarditis can lead to myocardial damage, heart failure, arrhythmias, and sudden death.The symptoms of myocarditis include fatigue, chest pain, shortness of breath, palpitations, fever, flu-like symptoms, and edema. However, some patients may not have any symptoms, or the symptoms may be mild and nonspecific. The diagnosis of myocarditis is based on the patient's medical history, physical examination, electrocardiogram (ECG), echocardiogram, blood tests, and imaging studies such as cardiac MRI or biopsy.
The treatment of myocarditis depends on the underlying cause and severity of symptoms. In viral myocarditis, antiviral drugs may be prescribed if the virus is identified. Immunosuppressive drugs such as corticosteroids or intravenous immunoglobulin (IVIG) may be used to suppress the immune system if there is evidence of autoimmune myocarditis. In severe cases, mechanical circulatory support or heart transplantation may be necessary.
Can COVID-19 lead to myocarditis? Almamlouk et al performed a systematic review of 50 autopsy studies and 548 hearts of patients who died of or with COVID-19. Usual post-mortem findings of tissue edema and necrosis were reported commonly. About two thirds of hearts had SARS-CoV-2 found in the tissue. However, none of the hearts had extensive myocarditis as the cause of death.
The symptoms of endocarditis include fever, chills, fatigue, night sweats, weight loss, arthralgia, myalgia, anorexia, abdominal pain, and new or changing heart murmurs. The diagnosis of endocarditis is based on the patient's medical history, physical examination, blood tests, echocardiogram, and imaging studies such as CT or MRI.
The treatment of endocarditis involves antibiotics to eliminate the infection, and in some cases, surgery may be required to repair or replace the damaged valve. The choice and duration of antibiotics depend on the type of organism causing the infection, the severity of symptoms, and the presence of complications such as abscesses or emboli.
Endocarditis is often characterized by systemic symptoms such as fever, chills, and weight loss, as well as new or changing heart murmurs, which are not typically seen in pericarditis or myocarditis. The diagnosis of all three conditions involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Treatment varies depending on the underlying cause and severity of symptoms.
Endocarditis
Endocarditis is the inflammation of the endocardium, the inner lining of the heart chambers and valves. Endocarditis can be caused by bacterial, fungal, or rarely, viral infections, and it can affect both native and prosthetic valves. Endocarditis can lead to valve dysfunction, heart failure, embolic events, and sepsis.The symptoms of endocarditis include fever, chills, fatigue, night sweats, weight loss, arthralgia, myalgia, anorexia, abdominal pain, and new or changing heart murmurs. The diagnosis of endocarditis is based on the patient's medical history, physical examination, blood tests, echocardiogram, and imaging studies such as CT or MRI.
The treatment of endocarditis involves antibiotics to eliminate the infection, and in some cases, surgery may be required to repair or replace the damaged valve. The choice and duration of antibiotics depend on the type of organism causing the infection, the severity of symptoms, and the presence of complications such as abscesses or emboli.
Pericarditis vs Myocarditis vs Endocarditis: Differences and Similarities
Pericarditis, myocarditis, and endocarditis all involve inflammation of the heart, but they affect different layers and structures. Pericarditis affects the pericardium, myocarditis affects the myocardium, and endocarditis affects the endocardium. Pericarditis and myocarditis can have similar symptoms such as chest pain, shortness of breath, and fatigue, but pericarditis is typically associated with sharp, stabbing pain that worsens with deep breathing, while myocarditis may be asymptomatic or present with nonspecific symptoms.Endocarditis is often characterized by systemic symptoms such as fever, chills, and weight loss, as well as new or changing heart murmurs, which are not typically seen in pericarditis or myocarditis. The diagnosis of all three conditions involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Treatment varies depending on the underlying cause and severity of symptoms.





.png)


Comments
Post a Comment