Proton Pump Inhibitors May Increase Dementia and Stomach Cancer Risk: Studies (2024)
Proton pump inhibitors (PPIs), a popular class of heartburn drugs, are linked to stomach cancer, a 2024 review found.
The review indicates that prolonged use of PPIs—exceeding three months—“is significantly associated with an elevated risk of cancer,” while shorter-term usage “appears to pose a comparatively lower risk,” the authors wrote.
PPIs are potent drugs that lower stomach acidity. They work by binding irreversibly to proton pumps—proteins in the stomach that release protons, a component of stomach acid. This action prevents the secretion of protons.
These acid reflux and ulcer drugs could significantly increase the risk of dementia when taken for a long time, a 2023 research suggests.
The findings, published in Neurology, ring alarm bells for the more than 15 million Americans prescribed PPIs—the most common of which are esomeprazole (Nexium), omeprazole (Prilosec), and lansoprazole (Prevacid)—to treat their chronic gastric woes.
“Although PPI are generally considered to be effective and safe, they have many potential risks,” the study authors noted. They also recommended that the drug be used at the lowest possible dose and only briefly.
Risk Observed Only With Long-Term Use
The study analyzed 5,712 people over 45 (average age 75) without dementia symptoms. Researchers reviewed medications during study visits and annual phone calls, finding 1,490 people, or over one-quarter, used PPIs.
Participants were split into four groups: nonusers, short-term users (around three years), users who took them between 2.8 and 4.4 years, and long-term users (over 4.4 years). Over 5.5 years, 10 percent developed dementia. Of the nonusers, 415 developed dementia. Of long-term PPI users, 58 developed dementia.
After adjusting for factors like age, sex, race, blood pressure, and diabetes, use over 4.4 years was linked to a 33 percent higher dementia risk versus nonusers. No increased risk was seen with short-term use.
Patients should talk to their doctors before changing medications, as stopping abruptly could worsen symptoms, Kamakshi Lakshminarayan, who holds a doctorate in cognitive science and is a coauthor of the study, told The Epoch Times, emphasizing that the study showed an association, not causation.
There are several notable limitations of the research.
Medication use was self-reported once a year, possibly missing nuances. Also, over-the-counter (OTC) PPI use wasn’t assessed. OTC formulations are often at a lower dose than prescription PPIs, Dr. Henry Jen, who specializes in advanced gastroenterology at Northwell Long Island Jewish Forest Hills in New York and is not involved in the study, told The Epoch Times.
But Short-Term Use May Have Risks, Too
Adding to evidence of cognitive risks with PPIs, a small 2015 study found even short-term use may impair function.
The research randomly divided 60 volunteers into six groups; five tested different PPIs (omeprazole, lansoprazole, rabeprazole, pantoprazole, and esomeprazole), while one was a control.
All groups took five computerized neuropsychological tests of the Cambridge Neuropsychological Test Automated Battery—once at the beginning and once a week after the end of the study.
The findings showed “statistically and clinically significant impairment in visual memory, attention, executive function, and working and planning function” among PPI users versus the control group.
“All the PPIs have some exacerbated effects on cognition,” the authors concluded. Though these adverse effects may go unnoticed initially, long term, they may contribute to Alzheimer’s disease development, they added.
PPIs May Cause Nutrient Deficiency, Affecting Cognition
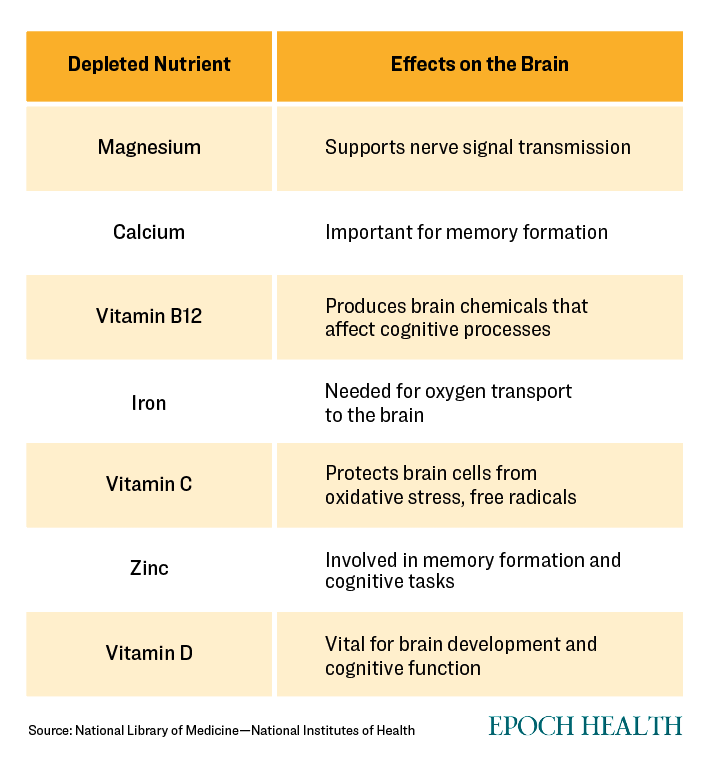
Antacid drugs can deplete levels of several vitamins and minerals crucial for brain health, including vitamin B12, vitamin C, calcium, iron and magnesium.
“While these risks are considered to be relatively low in the general population, they may be notable in elderly and malnourished patients, as well as those on chronic hemodialysis and concomitant PPI therapy,” the study authors noted.
B-12 supplementation may only be effective if started before neuron damage begins in middle age, according to some research.
Alternatives to PPIs
While some conditions, like Barrett’s esophagus, where the esophagus becomes damaged by acid reflux, or hyper-secreting tumors, necessitate PPIs, these drugs are often over-prescribed and overused unnecessarily, Dr. Jen said. “Especially long-term.”Potential health risks could be reduced by constantly reevaluating the need for PPIs and discontinuing them if no longer beneficial, he added.
Lifestyle changes can also minimize symptoms, including losing weight, avoiding food triggers and late snacking, and elevating the head in bed. “These modifications can often reduce or eliminate the need for PPIs,” Dr. Jen said.
Non-drug options may include surgery or newer endoscopic procedures like transoral incisionless fundoplication (TIF). This minimally invasive treatment reinforces the muscle between the esophagus and stomach to prevent reflux without surgery.
Dr. Scott Rollins from the Integrative Medicine Center of Western Colorado told The Epoch Times that while PPIs can be highly effective in controlling a potentially dangerous stomach ulcer in these patients, they may have cumulative adverse effects.
Dr. Rollins has found that many patients complaining of GERD often have unaddressed inflammatory gut problems. Once these problems are addressed by improving diet for six to 12 weeks, GERD symptoms tend to resolve or improve significantly, such that patients only need to take antacids.
He also pointed out that while heartburn is often treated by reducing stomach acid, counterintuitively, it may occur due to insufficient stomach acid, which can occur due to old age, thyroid problems, and a type of stomach autoimmune disease.
Between the esophagus and the stomach is a ring of muscle known as the lower sphincter. This sphincter is the opening of the stomach and is responsible for closing it to prevent undigested food and stomach acid from backflowing up the esophagus.
Heartburn occurs when the sphincter does not close properly. Acid and food return to the esophagus, causing pain and damage.
Several things can cause the sphincter to malfunction. One is that the stomach acid’s pH is not low enough. Therefore, while PPIs may reduce the symptoms, they may actually be counterproductive.
Other factors that can affect the sphincter include alcohol, caffeine, and smoking. Being overweight can also put more pressure on the stomach, leading to acid reflux.
Sources:
https://www.theepochtimes.com/health/heartburn-medication-may-increase-dementia-risk-5457912

.png)



.png)

Comments
Post a Comment