Crucial Facts About Your Metabolism (2024)
- Cortisol is primarily a rescue hormone. It's a glucocorticoid, so it increases your glucose level by shredding your muscle protein to produce glucose. Cortisol also accelerates the aging process and is implicated in most chronic diseases. It also uses your brain tissue to use amino acids to make glucose which contributes to brain atrophy and subsequent depression
- Your mitochondria can only burn one fuel at a time — either fat or glucose — and there’s a stealth switch that controls which of these fuels your mitochondria will burn. This switch is known as the Randle cycle
- Ideally, you want to metabolize (burn) glucose in your mitochondria, as this only generates 0.1% reactive oxygen species (ROS). This route also generates energy most efficiently, creating 36 to 38 adenosine triphosphates (ATP) for every molecule of glucose that is metabolized. For this to occur, you need to consume less than 30% of your calories as fat
- When you consume significantly more than 30% fat, the switch changes to burn fat in your mitochondria. As a result, glucose then backs up into your bloodstream, raising your blood sugar. This is a major contributor to diabetes
- When you lose muscle, your basal metabolic rate goes down, so it’s important to maintain muscle mass, because your muscle will burn fat even when you’re resting
Despite having a degree in computer science and having no formal academic training in health, Dinkov essentially has acquired a Ph.D. in molecular biology. After graduating from Georgetown University in 2002, Dinkov got a job as a programmer at the National Biomedical Research Foundation (NBRF).
There, he helped develop uniprot.org, a database of all known protein sequences. Surrounded by dozens of the brightest doctors and biochemists in the world, he developed an interest in biochemistry.
Low-Carb, High Fat Diet: Clearing Up Confusion
I have long promoted a low-carb, high-fat diet for many years and have realized many are confused on the evolution of my recommendations. As I say in the interview, 95 to 97% of the population in the U.S. is metabolically inflexible and would likely benefit from a low-carb, high-fat keto approach with intermittent fasting.However, once you have resolved your insulin resistance, which typically takes a few months but can take longer, and can optimally burn fat for fuel, it is very clear to me that you need to cycle carbs back into your diet. There are loads of questions about how this transition occurs, the timing of the transition, and the details of the cycling that need to be answered.
No one knows the answers, as the studies have not been done, but I am fairly convinced that many people will appear to do well in the long term on a low-carb, high-fat keto program like I did. However, I also believe they would do even better if they started to include more healthy carbs in their diet like I did. That does not mean processed foods or processed sugars, or virtually all grains and legumes. The ideal carbs are ripe fruits.
You should introduce carbs slowly and only after you have shifted your fat level down to 30%. This is easily calculated by using a free online program called Cronometer. If you still struggle with diabetes or obesity, then you can get your fat level down to 15 to 20% of your total calories.
Protein level should always remain the same and does not change from 0.7 to 1 gram protein/kg of lean body weight. So, if you are 20% body fat then you would multiply your body weight by 0.8 to get your lean body mass.
In my case, it took me about three to six months to go from 100 grams of carbs to 500 grams. The results for me were quite spectacular. I was already healthy, but it clearly improved my health even further as my body fat dropped from 15% to 12%, my inflammation decreased to radically low levels as my HS-CRP went from 0.8 to 0.18 which is almost below detection levels. Finally, even though I was not prediabetic as my blood sugar was in the low 90s, it dropped by 10 points to the low 80s.
The reason I made this shift is I was overwhelmed by the amount of strong scientific support for demonstrating that the ideal fuel in your mitochondria is indeed glucose, not fat. It has to do with decreasing reductive stress in your mitochondria which is a relatively unknown concept in molecular biology.
When implementing the transition to healthy carbs you need to be careful not to eat too many carbs as excess carbs will be shunted to glycolysis and into glucose into your blood and lead to an increased blood sugar. The more muscle mass you have and the more exercise you do, the more carbs you can eat.
I suspect most people could easily transition to 200 grams of carbs. I seem to do well with about 500 grams, mostly all fruit but do have white rice and red potatoes as well. You should see my shopping cart as every week it is loaded with about 60 pounds of fruit.
The Cortisol-Glucose Link
For example, Dinkov helped me understand the crucial role cortisol plays in glucose regulation. Cortisol is primarily a rescue hormone. It's a glucocorticoid, and as the name implies, it increases your glucose level, because if your glucose level drops too low, you will go into a hypoglycemic coma and can die.As such, cortisol is a lifesaver. The downside is that it uses up vital protein to make glucose, so high cortisol takes a toll on your muscles. The reason anabolic steroids build muscle mass is because they’re anti-cortisol. You would've thought anabolic steroids would have some direct action on the muscles, but no, they primarily inhibit cortisol’s catabolic impact.
Cortisol uses muscle protein to produce glucose in your liver, so when your glucose level drops, cortisol rises and shreds muscle to produce glucose. This is one of the puzzle pieces that explains why you don’t want your glucose levels to be low over prolonged periods.
Cortisol also accelerates the aging process and is implicated in most chronic diseases. In the case of Addison’s disease (adrenal failure), the opposite is present: low cortisol. These patients are typically required to take cortisol injections on a regular basis. On the upside, this chronic cortisol deficiency tends to impart a youthfulness. In most other chronic conditions, high cortisol is part of the problem.
High Cortisol Speeds Aging
Dinkov comments:You can do that either by injecting synthetic or natural glucocorticoids, or by increasing the levels of natural anti-cortisol steroids in the body. Those are progesterone and DHEA, and in males testosterone and dihydrotestosterone.
It has been shown that cortisol levels do not decline with age unless you really have adrenal failure, while the levels of all these anti-cortisol, youth-promoting hormones decline with age. By the time you're 80, their levels are at about 20% of what they used to be when you were in your 20s.
So, really, what happens is that cortisol stays the same, but your relative state of cortisol increases because there's nothing to oppose the cortisol that is already there. Multiple intervention studies have demonstrated that if you administer agents that oppose cortisol, block it at the receptor level, or reduce its synthesis, you can achieve really good health results and also improve the way you look.
Anabolic steroids are probably the best known example. It's really a misnomer because they're not anabolic. They're actually anticatabolic. Muscle has one of the highest expressions of the glucocorticoid receptor, through which cortisol shreds the muscle. It binds the receptor and increases a number of different proteolytic fibers.”
High Cortisol Linked to Depression
Your gastrointestinal tract and brain also have high numbers of glucocorticoid receptors, so cortisol shreds brain tissue as well, causing brain atrophy and subsequent depression. Research has shown that people with depression have smaller brain volumes than people who don't have depression.
“Within 48 hours of the glucocorticoid blocker RU-486 being administered to people with clinical treatment-resistant depression, they experienced remission. So I think it's a very good argument that cortisol is catabolic to the brain, and clearly, if it's catabolic to the brain, it's probably not going to improve your mood. If anything, it's going to worsen it.”Again, when your blood sugar level drops, that triggers your body to increase cortisol, which is the last thing you want if you struggle with depression or other chronic disease. Really, one of your primary goals in achieving optimal health is to limit the elevation of your cortisol. It’s far more destructive than having elevated blood sugar, which most focus on.
High Cortisol Is Far Worse Than High Blood Sugar
Many wear continuous glucose monitors that check your glucose level every five to 10 minutes. But high glucose is not the real danger here. Cortisol is, and it rises when glucose drops too low. As noted by Dinkov:
“All the drugs on the market, especially the more recent ones that lower HB A1C, the glycated hemoglobin, all of them increase mortality. So, clearly, messing directly with the levels of blood glucose, it's not something you want to do.You may temporarily decrease the biomarker, the glycated hemoglobin, but it does not mean you're getting healthier. [These drugs] may lower your blood glucose, but they may kill you in the long run faster than the elevated glucose would've done by itself.”
Metformin is one classic example. Many are using this drug to lower their blood sugar. While it’s a natural product, and considered safe, it’s basically a mitochondrial toxin that will make your health decline in the long term.
All of that said, we’re NOT saying you should ignore elevated blood glucose. Absolutely not. But elevated glucose is a symptom that is best addressed indirectly. Once you address the foundational cause, it will normalize by itself. As a personal anecdote, when I first interviewed Dinkov, 70% to 80% of my diet was fat. Now, I’m down to 27% fat and 57% carbohydrates, and I’ve lost 5 pounds and my fasting blood sugar is down by 10 points.
So, it's not the carbohydrate ingestion that’s causing high blood sugar. It's what's happening at the mitochondrial level. To help you understand that, I created a graphic (below) because this science can get somewhat complex.
The Randle Cycle
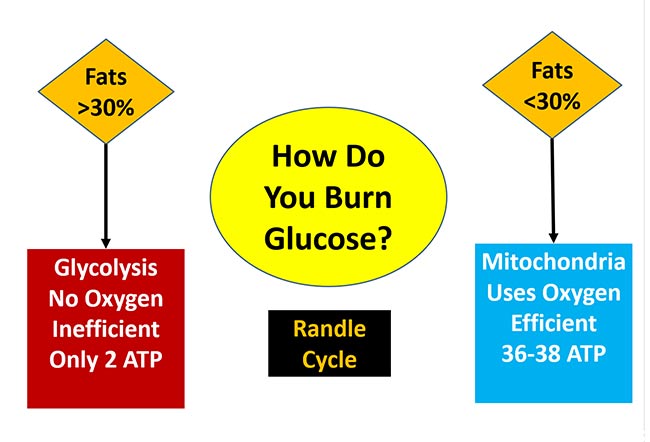
Your mitochondria can only burn one fuel at a time — either fat or glucose. Fats are broken down in a process called beta oxidation into acetyl-CoA, which gets fed into the Krebs cycle. Carbs are broken down to pyruvate, which cannot enter the electron transport chain until it is converted to acetyl-CoA by pyruvate dehydrogenase.
The key here is that there’s a stealth switch that controls which of these fuels your mitochondria will burn. The switch has been given the name the Randle Cycle, but it is more helpful to visualize it as a railroad switch that changes the tracks of the train. The train can only travel down one track: not both. This is because only one type of fuel can be burned at a time.
In a best-case scenario, you will metabolize, or burn, glucose in your mitochondria without any reductive stress. When you do this, you will only generate 0.1% reactive oxygen species (ROS).
Not only does this route generate less ROS, but it also is incredibly efficient at energy production by creating 36 to 38 adenosine triphosphates (ATP) for every molecule of glucose that is metabolized. It will also generate metabolic water and carbon dioxide, which are also important for your health.
For this to occur, as indicated in the figure above, you will need to consume less than 30% of your calories as fat. When you consume significantly more than that amount, the switch changes to burn fat in your mitochondria and you will not be able to burn glucose until your fat decreases to less than 30% of calories.
When your fat intake is higher than 30%, pyruvate is inhibited and unable to readily convert the glucose metabolite, pyruvate, into acetyl-CoA to be shuttled into the mitochondria to burn as fuel.
Consequently, glucose can back up into your bloodstream, raising your blood sugar. What little glucose is burned for fuel is done through glycolysis, which is a primitive pathway that bacteria and cancer cells use, and it generates the powerful metabolic reductant lactate.
This can be a major contributor to diabetes. If you’re exercising, healthy and doing strict keto, overt diabetes is unlikely to develop, but more than likely you will have fasting glucose in the 90s, rather than the more optimal 80s.
Additionally, chronically oxidizing fats as your primary fuel will tend to increase your cortisol level, resulting in chronic inflammation, both of which accelerate the aging process due to excess ROS generated in the mitochondria that occurs from increased reductive stress as a result of oxidizing fat instead of sugar.
It is great that we have this glycolysis pathway, as you absolutely need it for quick fuel when you are activating your Type 2 muscle fibers. But if this is the primary way you burn glucose, you are in a catastrophic metabolic state because you’re creating loads of lactate as a waste product instead of healthy CO2 and metabolic water.
What’s more, you’re only generating two ATP for every molecule of glucose, which is 95% less energy. Lactate increases reductive stress, which causes reverse electron flow in the mitochondria and increases the ROS to 3% to 4%, which is 30 to 40 times more than when glucose is burned efficiently in the mitochondria at 0/1% ROS.
When Adding Carbs, Reduce Your Fat Intake
Ideally, it is best to lower your fat intake and replace those calories with healthy carbs like ripe fruit. You likely won’t optimize your mitochondrial function, though, until your fat level decreases to 30% of your total calories. So, hold off on making a final decision about whether this change is helping you or not until you get your fat level to 30% or lower.
This is easily calculated by using a free online program called Cronometer. If you still struggle with diabetes or obesity, then you may need to get your fat level down to 15% to 20% of your total calories.
Protein Versus Fat and Carb Requirements
Determining the ideal balance between carbs and fats is the primary challenge for most people. The level of protein is a bit simpler. It tends to be about 15% of daily calories and remains stable. A basic guideline for protein intake is somewhere between 0.7 grams and 1 gram per kilogram of lean body mass (not total weight).
The level of dietary fat you need will depend on your endocrine balance. If you’re diabetic, for example, you may need to go below 20% to avoid shutting down your glucose metabolism. Dinkov comments:
“If you look at older people, and sick people as well, they have metabolic inflexibility. So, if you give them a meal that's comprised of equal number of calories of carbs and fats, they're going to oxidize mostly the fats and the carbohydrates will go unmetabolized.So, they'll raise their blood glucose and lactate. So, you need to play with the ratio, but I've noticed that between 15% and 20% is probably where most people in their current health state can metabolize the fat without causing problems through the Randle Cycle.
Most diabetics are overweight ... which means they have plenty of supply of fat. In fact, they have two sources of fat: one through the diet, and the second one from their fatty tissue, because there's always some lipolysis going on, which means shredding the fatty tissue and supplying the rest of the body with the fatty acids from a fatty tissue ...
In the rested state, your muscles actually prefer to oxidize mostly fat. So, if you have a decent amount of muscle mass, you can actually burn most of this fat through the baseline lipolysis by simply resting and preferably raising the amount of lean muscle mass you have. The ratio of lean muscle mass to total body weight is the primary determinant of your basal metabolic rate. So it's very important to not lose lean muscle mass ...
So, for diabetic people, it’s probably a good idea to lower the intake of fat from the diet because they already have a lot coming from their own bodies. In fact, there are many clinics around the world that treat and even cure Type 2 diabetes by putting diabetics on this really restrictive diet until they lose most of their fat and then suddenly the metabolism of glucose gets restarted.
I think this directly shows you that it wasn't the glucose that was fattening them up and causing the problems, rather they had too much fat in their bodies. Once you get rid of that fat, no matter how you do it ... the problems with metabolizing glucose disappear.”
Signs of Excessive Fat/Insufficient Carb Intake
As explained by Dinkov, one of the reasons why obese people who lose a lot of weight end up gaining it all back, even when they continue to diet and exercise, is because most of the weight lost is actually muscle mass. When you lose muscle, your basal metabolic rate decreases, meaning you need fewer calories to maintain your weight.
As a result, you must stay on an extremely low-calorie diet to maintain your weight. So, again, it’s crucial to maintain muscle mass, because your muscles will burn fat even when you’re resting. During activity, especially strenuous activity, your muscles will burn mostly glucose.
“I think the best way to gauge if you are eating too much fat is cognitive function,” Dinkov says. “If you're eating too much fat, to the point where you're interfering with glucose metabolism, you'll start getting brain fog. Your thinking process will slow. You'll start searching for words. Your reaction time and coordination time will decrease.Sleep quality is another. Also, exercise capacity. If you're always catching your breath and you're feeling fatigued all the time, that is actually a great sign/symptom of elevated lactate. In fact, many different interventions that lower lactate are used as performance improving substances, such as vitamin B1 and niacinamide ...
I would say eat the more fat-heavy meals earlier in the day, for breakfast and maybe lunch, and then eat the more carb-heavy meals at night, because your brain and many of the other organs will really need that.
It's very common that if you don't consume sufficient amount of carbs before going to bed, you will have trouble sleeping ... I think one of the reasons for this is that, if you don't consume sufficient amount of glucose, you will raise cortisol at night, and cortisol is already higher at night than it should be.
The cortisol is lowest at around 3 or 4 p.m. and starts rising with the coming darkness. Cortisol is highest at around 6 to 8 a.m. in the morning. But if you don't consume a sufficient amount of carbs, that cortisol will be up to 40% higher.”
Clean Carbs
Of course, when we say “eat more carbs,” we don’t mean pizza and doughnuts or even ostensibly healthy grains like whole wheat. Healthy or “clean” carbs include foods like ripe fruit, raw honey and maple syrup. Tropical fruits such as papaya, watermelon, oranges and tangerines are preferable, as in addition to higher levels of fructose, they also contain flavonoids that help to digest the sugars. Ripe melon, apples, peaches, plums, pears and grapes are also good.
Now, you’ve probably heard me say that you shouldn’t eat anything at least three or four hours before bedtime to optimize autophagy. Dinkov’s research, however, dispels some of the concerns about eating (clean) carbs before bed.
“You do not want to mess with autophagy too much,” Dinkov says. “It has a lot of beneficial effects in terms of getting rid of dead or metabolically deranged tissue. However, if you do have an already present tumor, autophagy and AMPK can actually drastically increase its aggressiveness and promote metastasis.But let's say you do want to increase autophagy. I think it's a bit of a myth that eating will somehow suppress autophagy and put it at a suboptimal level. Several studies demonstrate that several of the carbohydrates — including fructose and sucrose — are autophagy enhancers.
I would say, [eat healthy carbs] an hour before bed, because if you eat a meal that's too high in carbohydrates, there's the infamous fructose malabsorption. There's only a certain amount of carbohydrates that your gastrointestinal tract can absorb per unit of time.
So, you need about an hour or two before the meal, if it's composed of simple carbohydrates, to get these things into your bloodstream. At that point, you'll probably be very relaxed and naturally inclined to fall asleep.”
That fructose and sucrose enhance autophagy is probably news to most of you. It was to me. I personally eat a teaspoon of honey before I go to bed, which seems to be enough carbs to thwart an increase in cortisol and helps me get more deep sleep. So, to summarize, Dinkov suggests eating a small amount of healthy carbs, such as fruit, about an hour or two before bed to optimize sleep and, potentially, autophagy as well.
Serotonin Is Not Your Friend
Fruits to be consumed in small amounts include pineapple and bananas, as both contain serotonin. Bananas also contain tryptophan, which is used in the synthesis of serotonin.
While most people think of serotonin as a mood-booster, it’s actually one of your worst enemies. You do not want high levels of serotonin, because it’s an antimetabolite. This means it suppresses your body's ability to create energy in your mitochondria in the electron transport chain, so you become tired and fatigued, your metabolic rate slows and you gain weight.
“The amount of serotonin we need is really, really low,” Dinkov says. “The biggest role of serotonin is gastrointestinal motility. Any increase, even minor increase of serotonin, has been known since the 1920s to rapidly lead to fibrosis. The most successful antifibrotic drugs on the market currently are serotonin blockers.”

.png)




.png)
Comments
Post a Comment