Peter Attia Outlive Review 2023

We live in a golden age of health nuts, superfood gurus, exercise overachievers, and suspiciously young-looking longevity researchers. Yet for all this marketed youth, life expectancy is stagnant, scant progress has been made against the various dementias, and the average American keeps growing larger. Enter “geroscience,” the science of aging. In contrast with the generally poor popular discourse on the subject, physician Peter Attia’s new book, Outlive, written with journalist Bill Gifford, is a readable and wide-ranging primer to living a long life.
• Why the cholesterol test at your annual physical doesn’t tell you enough about your actual risk of dying from a heart attack.
• That you may already suffer from an extremely common yet underdiagnosed liver condition that could be a precursor to the chronic diseases of aging.
• Why exercise is the most potent pro-longevity “drug”—and how to begin training for the “Centenarian Decathlon.”
• Why you should forget about diets, and focus instead on nutritional biochemistry, using technology and data to personalize your eating pattern.
• Why striving for physical health and longevity, but ignoring emotional health, could be the ultimate curse of all.

About Dr Peter Attia
Attia first emerged from obscurity in 2011 as a charismatic advocate for ketogenic diets, later founding the Nutrition Science Initiative (NuSi) in 2012 with writer and journalist Gary Taubes (author of Good Calories, Bad Calories). NuSi was born of frustration with the general state of nutrition-science literature and, with $40 million from the John Arnold Foundation (which has a track record of funding metascience projects), promised to be the “Manhattan Project” of nutrition science. It ended up funding multiple diet studies, one of which tested the conventional wisdom about diets but could not confirm it; another that found inconclusive results; another that suggested that the conventional wisdom is wrong, at least with respect to fat accumulation in the liver; and another that, depending on one’s perspective, either confirmed or refuted conventional thinking.*Now ten years older and wiser, Attia has spent the last half-decade building a medical practice and podcast that vacillates from longevity science to archery and race-cars, just some of his many obsessions. Gone is the ketogenic-diet enthusiast; instead, he is candid about its disadvantages.
Attia starts the book by summing up what conventional medicine can treat well: “fast death", broken bones, infections, damaged organs, and serious injuries. The astonishing rise in life expectancy over the twentieth century is attributable mostly to our near-rout of infectious diseases, especially in infancy and childhood. Medicine has made substantial progress against heart disease (still the leading killer of adults in the U.S.) and diabetes and scored some partial victories against cancer. These impressive results, unfortunately, are marred by what Attia calls the “Marginal Decade”—the drop in quality of life that most elderly people experience in their seventies and eighties. Focusing on aging itself, the most important risk factor for all these diseases, would seem like a logical next step.
- Medicine 1.0 was the first era of medicine that lasted about two thousand years, exemplified by Hippocrates. Its conclusions were based on direct observation and guesswork.
- Medicine 2.0 is what’s mostly practiced now, and is mainly about dealing with the symptoms of disease.
- Medicine 3.0 is what Attia practices and advocates, but is rare. It deals with prevention by first understanding the seminal causes of the most pernicious and life-threatening chronic diseases that kill us, especially as we age.
How We Die in the Modern Era — The 4 Horsemen
Attia cleverly appropriates the “Four Horsemen of the Apocalypse” of biblical fame to represent the four chronic diseases, one of each — at least — has a good chance of killing us:
- Heart disease (aka atherosclerosis)
- Neurodegenerative diseases (aka Alzhimer’s and Dementia)
- Cancer
- Type 2 Diabetes
These four diseases tend to kill us slowly, because Medicine 2.0 waits till we’re close to the crisis stage until it intervenes. Attia relates several stories that underscore this reality, including his own, where well before middle age, and just after he swam the Catalina Channel in Southern California, the good doctor finds out that the roots of heart disease have firmly taken root.
To achieve longevity — to live longer and live better for longer — we must understand and confront these causes of slow death .
Living healthier, longer is to extend healthspan, and to do that necessitates delaying death from all four of the Horsemen. This is within the span of your control, but it requires consistent effort, for The Horsemen have one persistently powerful risk factor in common — age. As you grow older, the risk grows exponentially that one or more of the four diseases represented by the Horsemen has taken root in your body where it will steadily grow.
Of the four, heart disease is the most common instigator of death.
Heart disease and stroke (or cerebrovascular disease), which Attia lump together under the single heading of atherosclerotic cardiovascular disease, or ASCVD, is the leading cause of death, killing in 2020 an estimated 697,000 people in the United States; 1 in every 5 deaths (more than any other cause , including cancer), and 17.9 million people per year globally, accounting for at least 30% of all deaths worldwide.
Medicine 2.0 does not slow down the Four Horseman, and that’s the fundamental problem that Attia has with this “classic” practice of medicine. Using ASCVD as an example, the guidelines for managing cardiovascular risk are based on an overly short time horizon, compared to the timeline of the disease. It needs to be identified, prevented and treated much earlier than is typically done within the realm of Medicine 2.0.
Quoting professor Jay Olshansky of the University of Illinois at Chicago School of Public Health, Attia writes:
“We’re trying to attack heart disease, cancer, stroke, and Alzheimer’s one disease at a time, as if somehow these diseases are all unrelated to each other, when in fact the underlying risk factor for almost everything that goes wrong with us as we grow older, both in terms of diseases we experience, and of the frailty and disability associated with it, is related to the underlying biological process of aging.”
We need another approach, says Attia, and that’s the purview of Medicine 3.0.
Medicine 3.0 is characterized by a more personalized and proactive approach to healthcare. It emphasizes the use of advanced technology and data analysis to predict and prevent diseases before they occur. Medicine 3.0 also embraces the importance of lifestyle factors such as nutrition, exercise, and stress management in maintaining good, life-long health.
The 4 Horseman Ride the Insulin Path
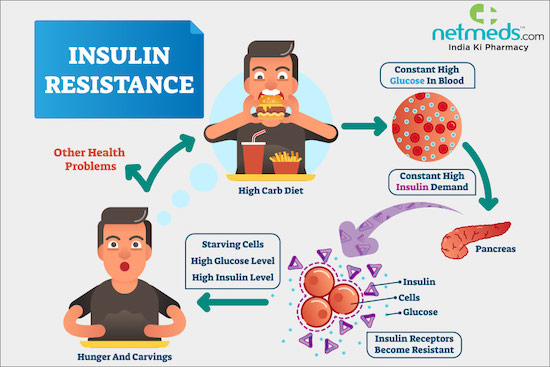
There’s a global epidemic of metabolic disorders that range from insulin resistance to type 2 diabetes. Insulin helps blood sugar enter the body’s cells so it can be used for energy, and signals the liver to store blood sugar for later use. When you eat food, your body converts that food into dietary sugars. Insulin is a hormone released by the pancreas that tells your cells to open up to that sugar and convert it into energy.
Insulin resistance is when cells in your muscles, fat and liver don’t respond well to insulin and can’t easily take up glucose from your blood. With insulin resistance, the cells don’t react, and don’t open up, resulting in excessive sugar in the blood. Over time, the pancreas keeps trying to regulate the blood sugar, producing more and more insulin until it wears out and can’t produce large amounts of insulin anymore. As a result, blood sugar levels increase to the point of being in the diabetic range.
Insulin resistance can lead to type 2 diabetes, but actually type 2 diabetes is a distinct disease clearly defined by various glucose metrics. Attia considers type 2 diabetes as “the last stop on a railway line passing through several other stations , including hyperinsulinemia, prediabetes, and NAFLD/NASH.” (NAFLD is nonalcoholic fatty liver disease, a condition in which excess fat builds up in your liver; and NASH, nonalcoholic steatohepatitis, is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver.)
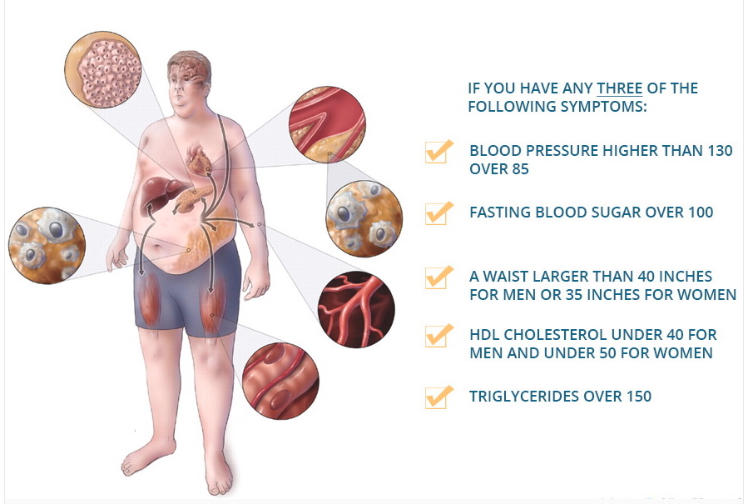
Once your body is resistant to insulin, you’re on the path to metabolic syndrome, which is defined as having three of the following five risk factors:
Attia reports that according to a 2020 article in JAMA (I don’t have the reference), about 90% of the U.S. population has at least one risk factor for metabolic syndrome, and “that nearly half of the population is either on the path to type 2 diabetes or already there.”
This concept of metabolic syndrome is valued by Attia, he says, because it helps identify these disorders as part of a continuum, as opposed to a single, binary condition. Medicine 2.0 routinely tests for these risk factors, if warranted, but is slow to respond until a person is well on his or her way of having three risk factors that indicate metabolic syndrome, or all five.
“Why wait until someone has three of the five markers?”, Attia asks, given that any one of them means that you’re sliding down a slippery slope to further health problems. A Medicine 3.0 approach would check for the warning signs years before there was a problem with the intention of intervening before a patient actually develops metabolic syndrome.
Attia lists a slew of biomarkers his clinic monitors related to metabolism, but the first thing he says he looks for, unsurprisingly, is elevated insulin. This for him is the “canary in the coal mine” of metabolic disorder, which is also ”associated with huge increases in one’s risk of cancer (up to twelvefold ), Alzheimer’s disease (fivefold ), and death from cardiovascular disease (almost sixfold) — all of which underscores why addressing, and ideally preventing, metabolic dysfunction is a cornerstone of my approach to longevity.”
Because people with diabetes have a much greater risk of cardiovascular disease, cancer, Alzheimer’s disease and other dementias, Attia argues that diabetes with related metabolic dysfunction is one thing that all these conditions have in common:
“This is why I place such emphasis on metabolic health, and why I have long been concerned about the epidemic of metabolic disease not only in the United States but around the world.”
Other metabolic-related topics discussed in Outlive
- Why humans have a unique capacity for turning calories from fructose into fat.
- Why fructose (ordinary sugar too) is a dastardly metabolic villain that even messes with the body’s production of ATP — cellular energy.
- Why you need to know about purines in certain meats, cheeses, anchovies, beer, etc., as well as uric acid (think gout).
- Why caloric restriction is a proven way to improve healthspan, and is connected to various cellular pathways, such as mTOR, AMPK and FOXO3.
- How the drugs rapamycin and metformin affect cellular pathways.
- How autophagy (cellular cleansing) is triggered by fasting, exercise and rapamycin.
The Cholesterol Story that Matters
Now, let’s turn to cholesterol. There’s lots here that you — and perhaps your doctor — does not know.
The cholesterol story is complicated, mainly because people haven’t kept up with the science about it, and because the only real important bits of it are rarely measured and considered.
First, it’s important to know that cholesterol is essential to life, given that it’s needed to produce some of the most important structures in the body, including:
- Cell membranes.
- Hormones such as testosterone, progesterone, estrogen and cortisol.
- Bile acids, which are necessary for digesting food.
Although all cells can synthesize their own cholesterol 20% of the supply made by our body is found in the liver, which you can visualize as a cholesterol repository of sorts that ships the cholesterol out to cells that need it and receives it back via blood circulation.
LDLs (low density lipoproteins) carry more lipids (think fats and oils), while HDLs (high density lipoproteins) carry more protein in relation to fat, and are therefore more dense.
Typically, when you go for your annual check up, your doctor orders a lipid panel that tests for LDL, HDL, total cholesterol and triglycerides (a type of lipid in blood). Once the results are in, you’ll be told that any of these measures are high, low or just right — but none of them really matter, because, as Attia dissects with precision, “it’s not the cholesterol per se that causes problems but the nature of the particle in which it’s transported.”
And that brings us to apoB.
Given the prevalence of heart disease — remember, it’s the world’s #1 killer — you must get your apoB tested, as I did a few months ago and was shocked by the result! This is because ApoB tests the aggregate of the LDL particles that cause atherosclerosis, and can lead to unhappy events like heart attacks.
Every single lipoprotein that contributes to atherosclerosis carries this apoB protein signature.
ApoB consists of:
- LDL – low density lipoprotein transports cholesterol from the liver to cells. 80% of its total weight contains lipids.
- VLDL – very low density lipoprotein transport triglycerides from the liver to adipose tissue. 91% of its total weight contains lipids.
- IDL – intermediate density lipoprotein are not usually detectable in the blood. Its size is between VLDL and LDL. 91% of its total weight contains lipids.
- LP(a) – Lipoprotein little a, an LDL with another special lipoprotein wrapped around it called apolipoprotein(a). This fella is the worst of all — it has an outsize ability to cause damage, even in relatively small numbers.
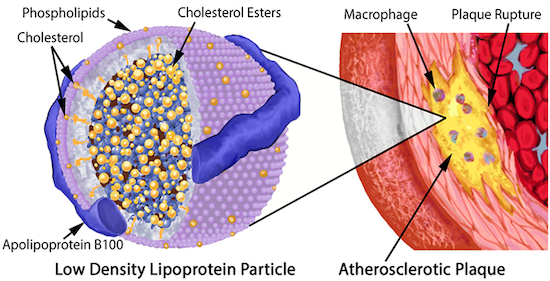
LDL particles become a problem when they begin to stick in the arterial wall and then become oxidized. This means the cholesterol (and phospholipid) molecules they contain come into contact with a highly reactive molecule known as a reactive oxygen species (ROS), the cause of oxidative stress. It’s the oxidation of the lipids on the LDL that kicks off the entire atherosclerotic cascade.
To discern your risk profile for atherosclerosis, the number of apoB particles circulating in your bloodstream must be determined. That number is much more relevant than the total quantity of cholesterol that these particles are carrying, not that the typical doctor practicing Medicine 2.0 will tell you that.
Medicine 2.0 has three blind spots when it comes to dealing with atherosclerotic disease, says Attia:
- First, it maintains an overly simplistic view of lipids that fails to evaluate the importance of total lipoprotein burden (apoB), and the necessity of minimizing it in order to truly reduce atherosclerotic risk.
- Second, a general lack of knowledge about apoB constituents, such as Lp(a).
- Third, a failure to fully grasp the lengthy time frame that encapsulates atherosclerotic disease progression, and the implications this carries if we seek true prevention.
Dr. Attia:
“ApoB not only tells me the concentration of LDL particles (which is more predictive of disease than the concentration of cholesterol found within LDL particles, LDL – C ), but it also captures the concentration of VLDL particles, which as members of the apoB family can also contribute to atherosclerosis. Furthermore , even someone whose apoB is low can still have a dangerously elevated Lp(a).”
So, you might wonder, how does all this cholesterol stuff actually cause atherosclerosis — a disease of the arteries characterized by the deposition of plaques of fatty material on their inner walls?
How atherosclerosis happens
Dr. Attia has vivid and detailed description of this processes that I’ll convey, inartfully, with a number of bullet points that provide the highlights:
- Aggregated or oxidized LDL on the artery wall instigates an immune response whereby macrophages (“big eater”) swallows it, but if it consumes too much of this cholesterol, they blow up into “foam cells”, so named because they look foamy under a microscope.
- When enough foam cells get together, they form a “fatty streak”, which is a precursor of an atherosclerotic plaque. (Teenagers typically already have some of these in their arteries.)
- The increasing number of foam cells begin to sort of ooze together into a mass of lipids, and become the core of our atherosclerotic plaque. In an attempt to control the damage, the “smooth muscle” cells in the artery wall migrate to this oozy waste site and secrete a kind of matrix in an attempt to build a kind of barrier around it, much like a scar.
- This matrix ends up as a new arterial plaque.
What can you do to slow down atherosclerotic progression?
You know the drill — get plenty of exercise, sleep, reduce stress, eat more plant food and much less processed meats and processed foods in general. But there’s two particular interventions that Attia explores that I want to spend a little time explaining:
- Reducing saturated fat, and
- Drugs.
Saturated Fat
Eating lots of saturated fat can increase levels of atherosclerosis – causing lipoproteins in blood, but Attia asserts that “most of the actual cholesterol that we consume in our food ends up being excreted out our backsides”, an assertion that Michael Greger, MD FACLM of Nutritionfacts.org contradicts.
In Attia’s clinical experience, about a third to half of people who consume high amounts of saturated fats (which sometimes goes hand in hand with a ketogenic diet) will experience a dramatic increase in the much unwanted apoB particles.
The reason for this is that (a) it appears that saturated fat contributes directly to the synthesis of excess cholesterol, and, more importantly, (b) excess saturated fat causes the liver to reduce expression of LDL receptors, thereby reducing the amount of LDL removed from circulation.
What we want is to increase apoB clearance by enhancing the body’s ability to get apoBs out of circulation. In large part, this is done by amplifying the activity of LDL receptors in the liver, which absorb cholesterol from the bloodstream.
I think this is sufficient reason to read food labels to see how much saturated fat is contained in the foods you eat, and to reduce your consumption of meat, if that’s something you frequently eat. (Typically meat is high in saturated fat).
Drugs
As mentioned, Dr. Attia devoted himself to lowering his chance of getting some form of atherosclerosis after he learned that he was primed for it. He learned that he has a genetic propensity for heart disease, underscored by the number of deaths by heart attack in his family tree. For him, lifestyle interventions were necessary but insufficient, and so like so many millions of people, he needed a statin.
Statins inhibit cholesterol synthesis, prompting the liver to increase the expression of LDL receptors, resulting in more LDL taken out of circulation. They may have other benefits too , including an apparent anti-inflammatory effect.
People who have a high apoB score might need a PCSK9 inhibitor and/or a statin.
In the case of apoB, Attia says:“Once you understand that apoB particles — LDL , VLDL , Lp(a) — are causally linked to ASCVD [atherosclerotic cardiovascular disease], the game completely changes. The only way to stop the disease is to remove the cause, and the best time to do that is now.”
Exercise
Anyone who has spent even a bit of time reading about Dr. Attia or watching his interviews knows that his number one prescription for improving healthspan is exercise:
“More than any other tactical domain we discuss in this book, exercise has the greatest power to determine how you will live out the rest of your life.”
Looming above anything else discussed in Outlive, Attia asserts that exercise has the greatest power to determine how you will live out the rest of your life. An overwhelming amount of data underscores this point, and, in fact, even a minimal amount of exercise can lengthen your life by several years.
Consistent exercise delays the onset of many chronic diseases, and is effective at extending and improving healthspan: it can reverse physical decline and slow or reverse cognitive decline as well. The bad news is that 77 percent of the US population does not exercise. The good news is that just going from zero weekly exercise to just 90 minutes per week can make a big difference in your quality of life as an old person.
Here are some facts about exercise that Attia underscores that hopefully focus your attention:
- Going from zero weekly exercise to just 90 minutes per week can reduce your risk of dying from all causes by 14 percent.
- Study after study has found that regular exercisers live as much as a decade longer than sedentary people.
- VO2 max, is perhaps the single most powerful marker for longevity. (VO2 max represents the maximum rate at which a person can utilize oxygen.)
- Whether by measures of cardiorespiratory capacity or muscular strength, the fitter you are the lower your risk of death.
Attia cites the work of Dr. John Ioannidis, Professor of Medicine at Stanford University who has run side-by-side comparisons between drug and exercise studies and found that in several randomized clinical
trials, exercise-oriented interventions performed as well or better than multiple classes of prescription drugs at reducing mortality from coronary heart disease, prediabetes/diabetes and stroke.
This is why, suggests Attia, exercise acts like a drug at the biochemical level:
- Exercise strengthens the heart and helps maintain the circulatory system.
- Exercise improves the health of the mitochondria, the crucial little organelles that produce energy in our cells via ATP, the energy used by cells.
- Improved mitochondria (mitochondrial biogenesis) improves our ability to metabolize both glucose and fat.
- More muscle mass and stronger muscles supports and protects the body, and maintains metabolic health, because muscles consume energy efficiently.
- Exercise prompts the body to produce its own endogenous drug-like chemicals, such as cytokines that help strengthen the immune system and stimulate the growth of new muscle and stronger bones.
- Exercise helps generate a potent molecule called brain-derived neurotrophic factor (BDNF) that improves the health and function of the hippocampus, a part of the brain that plays an essential role in memory.
- Exercise helps keep the brain vasculature healthy, and it may also help preserve brain volume (important for reducing Alzheimer’s risk).
That begs the questions: Why and what type of exercise?
Well, as you would expect, Attia addresses those questions and more in three chapters of Outlive that primarily encompass:
- Cardiorespiratory fitness (its association with longevity),
- Muscular strength (its association with longevity), and
- Stability (its association with longevity).
Stability is the last chapter about exercise in his book, but I’m going to review some of what he says about it first, because it’s the first thing that’s needed in order to do various cardiorespiratory and strength training safely and effectively.
Stability: the Foundation for The Best Exercises to Live Longer

Dr. Attia addresses stability in his last chapter on exercise, after cardiorespiratory fitness and muscular strength, but I want to address it first, because you want to build the foundation. Irrespective of where he put this chapter in Outlive, Attia agrees:
“…I think of stability as the solid foundation that enables us to do everything else that we do, without getting injured. Stability makes us bulletproof.”
Think of stability as the innate “ability to harness, decelerate, or stop force”. A person that has developed stability can respond “to internal or external stimuli to adjust position and muscular tension appropriately without a tremendous amount of conscious thought.”
Stability enables our body to summon the necessary force safely to connect different muscle groups when needed with minimal risk of injury to joints,soft tissue, and our vulnerable spine. The aim is to be “strong, fluid, flexible, and agile as you move through your world”.
So, how do you develop stability?
You get help.
You can easily learn, say, to do a bicep curl by watching others, or getting some detailed instruction, because it’s a simple movement that can be self-corrected by watching yourself do the movement in a mirror. Many stability exercises, however, are not that easy; they can be subtle and nuanced, requiring exacting compound movements (multiple muscles and positions) that are difficult to observe in the mirror, and require sufficient self-awareness about your body’s movement patterns for correct application.
In Attia’s case, he is fortunate enough to have someone in his clinic who has expertly guided him in improving what he admits was a poor foundation of stability that was leading him to various injuries as he did his cardiorespiratory and strength training.

Dr. Peter Attia’s trainer, Beth Lewis, demonstrates a stand-to-sit mobility/stability drill. This is a screenshot from a video available to buyers of the book, Outlive.
What you could do is to find someone credentialed in dynamic neuromuscular stabilization (DNS), which aims “to retrain our bodies — and our brains — in those patterns of perfect movement that we learned as little kids”.
DNS encourages you to think of the abdomen as a cylinder, surrounded by a wall of muscle, with the diaphragm on top and the pelvic floor below. You inflate the cylinder with a deep inhalation that expands your chest, ribs, abdomen and back, as if they’re one big cylindrical balloon. Once this cylinder is inflated, you feel what’s called intra-abdominal pressure (IAP). When you learn to fully pressurize this cylinder via IAP, your movement pattern becomes more safe, because the cylinder stabilizes the spine.
Of course, your options are not limited to DNS. Another option is to be coached by a yoga teacher well versed in movement precision, or to be aided by a movement modality that is proven to help you gain stable movement patterns. Make sure that whatever modality you choose to help you become more stable and mobile involves breathwork.
You also need to think about your feet, says Attia:
“If the road to stability begins with the breath, it travels through the feet—the most fundamental point of contact between our bodies and the world.”
Foundational stability begins with your feet. Before you do any exercise where you’re on your feet, you must be aware of them and how they’re contributing to the stability (or not) of the movement. Attia spends a lot of time on this topic in Outlive, as he does with breathwork; suffice to say that your feet are the beginning of a chain of inter-connected links that move up from the feet to your ankles, knees, hips and spine.
You can get some idea about the importance of your feet for stability by checking your balance. Stand on one foot — can you balance for 30 seconds? Close your eyes while standing on one foot — can you balance for 15 seconds?Cardiorespiratory Fitness Keeps Your Ticker Ticking
Cardiorespiratory fitness encompasses both aerobic and anaerobic capacity:
- Aerobic means ‘with air’ and refers to the body producing energy with the use of oxygen. This typically involves any exercise that lasts longer than two minutes in duration. Continuous ‘steady state’, Zone 2 exercise is performed aerobically. Think 5 kilometer jun.
- Anaerobic means ‘without air’ and refers to the body producing energy without oxygen, which then constrains the exercise effort to just a few minutes or shorter. Think 100 meter sprint.
So, cardiorespiratory fitness requires training that encompasses long, steady state endurance work, such as jogging or cycling or swimming (Zone 2), and maximal efforts over shorter periods (typically four minutes or shorter), where VO2 max comes into play.
Good cardiorespiratory fitness is valuable in order to attain a high quality of life as you get older. A study published in 2020 by the Journal of the American College Cardiology that studied a cohort of 750,302 US male and female veterans aged 30 to 95 years came to the same conclusions as many other such studies:
- Cardiorespiratory fitness (CRF) is inversely associated with all-cause mortality (more fitness = less death)
- Traditional risk factors like chronic kidney disease, smoking, diabetes, atrial fibrillation, cancer, cardiovascular disease, hypertension and age all were independently linked to increased mortality risk — but none as strongly as cardiorespiratory fitness.
- Those in the extremely fit cohort had the greatest survival. The lowest mortality risk was observed in people with exercise capacity of 14.0 METs. (METS, metabolic equivalents: One MET is defined as the energy you use when you’re resting or sitting still per minute. I wrote METs and VO2 max here.)
Let’s take a look at what Dr. Attia has to say about Zone 2 and VO2 max training.
Zone 2 Training Builds A Strong Aerobic Baseline
Zone 2 is steady-state aerobics. A good way to know if you’re in Zone 2 is when you can still have a conversation despite the effort you’re producing, but you rather not, as opposed to anaerobic training where you can only muster short exclamations.
Zone 2 can be easy to do, even for someone who has been sedentary for a while, because, as mentioned by the talk test, it’s subjective. For some people, a brisk walk might get them into Zone 2; for those in better condition, Zone 2 necessitates walking uphill. Common Zone 2 training includes riding a stationary bike, or using an elliptical machine, or jogging.
In technical terms, Zone 2 is the maximum level of effort you can maintain without accumulating lactate. You will still produce lactate, but you’ll be able to match its production with its clearance. The more efficient your mitochondrial “engine,” the more rapidly you can clear lactate, and the greater effort you can sustain while remaining in Zone 2. (More about mitochondria here.) If you are “feeling the burn” in this type of workout, then we are likely going too hard, creating more lactate than we can eliminate.
In Outlive, Dr. Attia writes about San Millán, an assistant professor at the University of Colorado School of Medicine, who has conducted some valuable research about why healthy mitochondria is the key to athletic performance and metabolic health.
Mitochondria can convert both glucose and fatty acids to energy. This is special, because although glucose can be metabolized in different ways, fatty acids can only be converted to energy in the mitochondria. You want healthy mitochondria (mitochondrial biogenesis) for many reasons, one being to achieve “metabolic flexibility”.
Metabolic flexibility refers to the ability to use both fuels, fat and glucose, to produce energy for the body. Typically, someone working at a lower relative intensity (Zone 2/aerobics) will be burning more fat, while at higher intensities (VO2 max/anaerobics) they would rely more on glucose. The healthier and more efficient your mitochondria, the greater will be your ability to utilize fat — by far the body’s most efficient and abundant fuel source.
San Millán believes that metabolic flexibility is fundamental for athletes, but even more important for nonathletes, because:
- It builds a base of endurance for your life’s activities — riding your bike for miles, or playing with your kids, grandkids, or great-grandkids.
- It plays a crucial role in preventing chronic disease by improving the health and efficiency of your mitochondria,
Mitochondria are very plastic, meaning they can undergo morphological and functional changes in response to cellular demands. When you do aerobic exercise, many new and more efficient mitochondria are created through a process called mitochondrial biogenesis. At the same time, dysfunctional mitochondria get recycled via a process called mitophagy (which is like autophagy, but specific to mitochondria).
A person who exercises frequently in Zone 2 improves their mitochondria at each exercise session. The converse is true as well — non-exercisers lose mitochondrial health. Inevitably, Zone 2 training builds muscle, a strong mediator of metabolic health and glucose homeostasis.
Muscle is our body’s largest glycogen storage sink in the body. When you create more mitochondria, you substantially augment your capacity for using that stored fuel, rather than having it end up as fat or remaining in blood plasma. You don’t want glucose to remain in your bloodstream. Chronic blood glucose elevations damage our heart, brain, kidneys and many other organs. It also contributes to erectile dysfunction in men.
Attia asserts that while we are exercising our overall glucose uptake increases as much as one-hundred-fold over what happens while at rest. During exercise, the glucose uptake occurs via multiple pathways — the usual insulin-signaled path, as well as one called non-insulin-mediated glucose uptake (NIMGU), where glucose is transported directly across the cell membrane without the involvement of insulin. This explains why exercise, particularly in Zone 2, can be so effective in ameliorating both type 1 and type 2 diabetes:
“It enables the body to essentially bypass insulin resistance in the muscles to draw down blood glucose levels”.
OK, not that you’ve laced up your sneakers for some Zone 2 training, let me convey what Attia says about the equally important part of cardiorespiratory fitness — Vo2 Max
VO2 max Training Builds Capacity
VO2 max, is a strong contender for the single most powerful marker for longevity. Typically expressed in terms of the volume of oxygen a person can use, per kilogram of body weight, per minute, VO2 max represents the maximum rate at which a person can utilize oxygen.
Whereas high intensity interval training (HIIT) intervals are very short, typically measured in seconds, or under two minutes, VO2 max intervals are a bit longer, ranging from three to eight minutes (but usually four is the most) — and are a bit less intense. You can do this type of training by running, on a bike, on a stationary bike, treadmill, rowing machine, or an “assault” bike (my favorite).
One effective formula for these VO2 max intervals is to go four minutes at the maximum pace you can sustain for, say, four minutes (a hard but less than exhaustive effort), and then bring the pace down for an easy four minute recovery period until the next interval.
Do not do VO2 max training until you have built a solid Zone 2 foundation!
Here’s some stats to consider showing the value of improving your VO2 max:
✔ Those below average VO2 Max (between 25th and 50th percentile) are at double the risk of all-cause mortality compared to those who are in the top quartile (75th to 97.6%). Given that a smoker has a 40% greater risk of all-cause mortality (risk of dying at any moment), poor cardiorespiratory fitness carries a greater relative risk than smoking!
✔ Someone in the bottom quartile of VO2 max (i.e., the least fit 25 percent) is nearly four times likelier to die than someone in the top quartile—and five times likelier to die than a person with elite-level (top 2.3 percent) VO2 max. That’s stunning. These benefits are not limited to the very fittest people either; even just climbing from the bottom 25 percent into the 25th to 50th percentile (e.g., least fit to below average) means you have cut your risk of death nearly in half, according to this study.
The most accurate way to measure VO2 max test is by a maximal exercise test performed on a treadmill or bike while connected to a machine capable of analyzing your expired air. This test provides data on how much oxygen you use as you exercise and determines the maximal oxygen you can consume during exercise.
But there’s a formula that provides a useful approximation:
VO2 max = 15 x (HRmax/HRrest)
Calculate your resting heart rate by counting your heart heat (pulse at the side of your throat is often most discernible) while at rest (after you wake up or have been surfing the couch for an hour or more)
Calculate your maximum heart rate by the formula 220 – your age.
So, VO2 max for a 50 year-old with a resting pulse of 65 would be:
15 x [(220 – 50)] / 65 = 39
The downside of this formula is that your maximum heart rate may be more or less than what the formula predicts; mine is. The formula predicts that my maximum heart rate is 153 (220 – 67), but a recent treadmill test monitored by a cardiac technician put it at 168, which at a resting pulse of 50, gives me a VO2 Max of 50.
Returning to our example, is 39 a good VO2 max for a 50 year-old?
How trainable is VO2 max, you may ask?
Attia says that it’s possible to improve elderly subjects’ aerobic capacity by:
- About 13 percent over eight to ten weeks of training, and
- By 17 percent after twenty-four to fifty-two weeks.
He also cites a study that found that boosting elderly subjects’ VO2 max by 6 ml/kg/min, or about 25 percent, was equivalent to subtracting twelve years from their age. So, for that 50 year-old in the above example, he/she could become twelve years younger biologically by increasing his or her VO2 max from 39 to 45.
Now let’s turn to muscle, another piece of the fitness muscle you need to live long and strong.Muscular Strength, Another Key Longevity Exercise
By age eighty, the average person will have lost eight kilograms of muscle, or about eighteen pounds, from their peak. But people who maintain higher activity levels lose much less muscle, more like three to four kilograms on average.
This loss of muscle (muscle wasting) is called “sarcopenia”. A recent study of older British adults found that those with sarcopenia at baseline were nearly six times likelier to report having a low quality of life a decade later than those who had maintained more muscle mass.
Although the association between cardiorespiratory fitness and longevity has long been known, the impact of muscle on longevity has been understood only recently, and it’s significant. Dr. Attia also cites a ten-year observational study of roughly 4,500 subjects ages fifty and older found that those with low muscle mass were at 40 to 50 percent greater risk of mortality than controls (presumably a similar cohort, but with average muscle mass).
What’s also been recently revealed is that even though muscle is important, more significant is the strength produced by the muscle: Those with low muscle strength were at double the risk of death, whereas those with low muscle mass, low strength AND metabolic syndrome, had a 3 to 3.33 times greater risk of all-cause mortality.
Another elevated risk for dying before your time is instigated by a loss of bone density. Dr. Attia measures bone mineral density in every patient each year, looking at both of their hips and their lumbar spine bone density using a DEXA scan, because these are three regions are what is typically used to diagnose osteopenia or osteoporosis.
Why?
Well, in addition to the undesired mobility compromises caused by osteopenia and osteoprosis, there’s this thing called “falling and breaking your hip.” Up to one-third of people over sixty-five who fracture their hip are dead within a year.
Even if a person does not die from the injury, the setback can be the functional equivalent of death, because of the ensuing loss of muscle mass and physical capacity from being bedridden.
Avoid that by exercising.
Cardiorespiratory and strength training has a greater positive impact on healthspan by managing the severity of the chronic diseases associated with aging than the drugs specifically created for those diseases.How To Be A “kick-Ass” 100 Year-Old
One insightful perspective that Attia brings to the topic of fitness is his admonition to set your fitness goals today for what you want to be able to physically do in the future in your very old age. You need to “set a trajectory”, he says.
He refers to this as the “Centenarian Decathlon”. Just like the decathlete is not the best at any of the ten events in a decathlon, he or she is good at all of them. Similarly, you need not be great at stability, or Zone 2, or VO2 max training or strength training — but you need to be decent at all of them should you want to be fit in old age.
You want to plan your trajectory, or pathway forward, recognizing the inevitable physical degradation that happens during the aging process. The more you want to be able to physically do in very old age, the fitter you need to be now!
Cleverly, Attia uses retirement savings as an analogy. Just like you (hopefully) have put aside money every month into a retirement account so you can retire with enough money saved up to sustain yourself until you part company with this world, you want to also reach older age with enough of a “reserve” of muscle (and bone density) to protect yourself from injury and chronic disease, and allow the unfettered pursuit of activities that bring you joy and fulfillment.
Just as with investments, you do not want to scramble late in life to make up for lost time, time that you could have devoted to building up your reserve of fitness.
One of several examples Attia uses to make this clear is that of a person who wants to be able to pick up his or her grandchild or great-grandchild off the floor. Let’s say the child weighs 30 pounds. To lift her off the floor is equivalent to doing a squat holding 30 pounds in front of you (like a goblet squat), suggests Attia.
Now, maybe you can do that 30 pound squat now, say at age 40 or 50, but will you be able to do it 30 or or 40 years from now, given that — without appropriate training — your muscle strength will decline by about 8 to 17 percent per decade, accelerating with time (it’s not a linear decline)?
Probably not.
Consequently, in order to be able to pick up that 30 pound kid decades from now, you need to be able to squat with more than 30 pounds today — perhaps as much as 55 pounds now.
There are many other examples to consider; here’s two:
- To lift a twenty-pound suitcase above your head to plop it in the overhead airplane compartment when you are older means doing so with forty or fifty pounds now.
- To be able to climb four flights of stairs in your eighties means you should be able to sprint up those four flights today.
In every case, you need to be doing much more now, to defend yourself against the natural and precipitous decline in strength and aerobic capacity that you will undergo as you age.
In this regard, a useful mental exercise that Attia employs in his own life is to list what you want to be able to physically do at the tail-end of your life and evaluate what that means you need to be able to do today. (This is the trajectory). Given that just 24 percent of Americans meet the Physical Activity Guidelines for both aerobic and muscle-strengthening activity, says the CDC, the odds are you have some work to do.
If you’re thinking that the “Centurion Decathlon” is unattainable, know that thousands of elderly people are doing it, some literally.
There are several sports organizations and competitions for the elderly that allow them to remain active and competitive, pursue a sport they enjoy, and optimize their health. One such organization is the National Senior Games, also known as the Senior Olympics, which hosts senior athletes from the United States and Canada to participate in national competitions every other year. The minimum age of eligibility is 50 years old, with the oldest participants being over 100 years old.
According to the National Senior Games Association (NSGA), the 2019 National Senior Games had a record 12,100 registered participants. The 2022 National Senior Games had 11,938 athletes registered to compete, the third-highest number in National Senior Games history. The NSGA also reported that nearly 12,000 athletes aged 50 and over competed in 21 sports in five-year age divisions over 13 days of the massive multisport event in 2022.
Some examples of sport achievements by elderly athletes include 100-year-old Orville Rogers, who set a new world record in the 60-meter dash in the 100+ age group at the 2018 National Senior Games, and 103-year-old Julia Hawkins, who set a new world record in the 100-meter dash in the 100+ age group at the same event.
- Grip strength: how hard you can grip with your hands, which involves everything from your hands to your lats (the large muscles on your back). Almost all actions begin with the grip.
- Concentric and eccentric loading: apply this for all strength training movements — contracting the muscle (concentric) and lengthening it (eccentric) under control.
- Pulling motions: do this at all angles, from overhead to in front of you (pull-ups, rows, etc.), which also requires grip strength (e.g., pull-ups and rows).
- Hip-hinging movements: such as the deadlift and squat, step-ups, hip-thrusters, and single-leg variants of exercises that strengthen the legs, glutes, and lower back.
Rapamycin, Acarbose and Canaglifloxin
Attia describes the discovery of rapamycin, a striking illustration of serendipity and persistence in drug research. The story starts with a scientific expedition to eerie Easter Island, filled with giant stone heads; then we meet biochemist Suren Seghal, whose characterization of the drug’s anti-fungal activity made him hopeful that he had discovered a cure for athlete’s foot. Later, Seghal persisted with experimentation even after his old company was bought up. Apart from its proven utility in transplantation, kidney cancer, and in drug-eluting-stents, rapamcyin holds a more elusive potential: life extension. Unlike other compounds with promising effects that later fail to replicate (most infamously resveratrol), rapamycin has generated effects that have shown up in multi-center trials of mice at various ages of treatment onset. Similar results have been found in yeast and fruit flies; the drug is now being tested in companion dogs.Policymakers should take heed. From Italy to America, longer life expectancies without corresponding improvements in “healthspan”—the years one spends in the prime of one’s health—are challenging developed-world safety nets. Yet the National Institute of Aging (NIA) budget is small. In 2023, the operating plan for the NIH apportions about $4.4 billion to the NIA, while the National Cancer Institute alone receives about $7.3 billion. Yet many more people will grow old than will ever develop cancer. If, as geroscientists hope, directly treating aging (instead of age-related diseases) improves health span, then longevity science may help resolve this elder-care budget crisis.
Apart from more research into the basic biology of aging, some specific “mega-projects” in aging could easily absorb considerably more funding. For instance, the Interventions Testing Program (ITP), which rigorously tests various compounds on laboratory mice in three separate laboratories, has identified several that reliably extend mouse lifespan. Some, like rapamycin, acarbose, and canagliflozin, are already FDA-approved for humans, though for other conditions. Funding in-human studies for both aging and age-related diseases—as, for instance, some have already proposed for rapamycin and Alzheimer’s disease—and for promising off-patent drugs should be an NIA priority, especially since these generic drugs are unlikely to see substantial future investment from industry. Expanding the ITP’s capabilities by increasing the number of compounds and testing in combinations would be a natural complement to this effort. Another possibility would be adding exotic interventions such as partial reprogramming (which aims to restore youthful patterns of gene expression) to the ITP, which currently prioritizes interventions that can be delivered through diet.






.png)



.png)

Comments
Post a Comment