Periodontal Disease and Alzheimer's Connection: An Important and Overlooked Cause of Alzheimer’s
Researchers have long linked gum disease to a higher risk of Alzheimer’s disease. Research has revealed that inflamed, bleeding gums are the entry point for disease-causing bacteria to get into the bloodstream and trigger issues that can lead to dementia.
That means dentists could be a first line of defense against cognitive decline—if only more of them recognized that possibility.
Nearly half of adults above the age of 30 have gum disease, and 70 percent of those who are 65 and older have periodontal disease, according to the U.S. Centers for Disease Control and Prevention. That means this population has an important modifiable risk factor for Alzheimer’s.
The key bacteria involved is Porphyromonas gingivalis (P. gingivalis), a cause of chronic periodontitis. Recent research has revealed that P. gingivalis can make its way to the brain and cause neuroinflammation, which can contribute to Alzheimer’s.
P. gingivalis can produce gingipains, a class of enzymes, some of which are toxic and can cause gum inflammation. Gingipains are neurotoxic and particularly harmful to tau, a protein our brains need for normal neuronal function. In Alzheimer’s, which also affects memory and communication, tau proteins begin to stick to one another, forming threads called neurofibrillary tangles that block the neuron transport system and harm communication between neurons.
The changes in an Alzheimer’s patient’s brain are suspected to come about because of these abnormal tau, beta-amyloid proteins, and other factors, according to the National Institute on Aging. Abnormal tau accumulates in brain regions involved in memory, and beta-amyloid forms clumps of plaque between neurons.
Gingipains Inhibitors
“Neuroinflammation induced by P. gingivalis has increasingly been recognized as a factor in the pathogenesis of AD [Alzheimer’s disease],” notes a 2021 review published in Frontiers of Neuroscience by Dr. Ingar Olsen, a microbiologist and dentist with the department of oral biology at the University of Oslo in Norway.
Dr. Olsen looked at previous research to dig deeper into how this neuroinflammation contributed to Alzheimer’s disease pathogenesis. He noted that P. gingivalis and gingipain have been detected in the brains of Alzheimer’s patients, and P. gingivalis DNA has been found in the brains and cerebrospinal fluid of patients. P. gingivalis lipopolysaccharide, a large pathogenic molecule, has also been detected in the brains of people with Alzheimer’s disease.
An animal study published in Science Advances in January 2019 had already concluded that P. gingivalis could cause Alzheimer’s disease by showing that negating the bacteria’s influence could prevent the disease.
In the study, researchers were able to block the bacteria’s neurotoxicity with synthesized small-molecule inhibitors targeting gingipains in mouse brains. The outcome was reduced P.gingivalis, blocked beta-amyloid protein production, reduced neuroinflammation, and rescued neurons in the hippocampus.
While it’s undoubtedly a great discovery, rodent research doesn’t always translate into human success. That study was funded in part by Cortexyme Inc., which went on to test its gingipain inhibitor, called atuzaginstat, in humans. It was eventually put on hold by the U.S. Food and Drug Administration due to liver toxicity concerns.
An Overlooked Warning
The link between Alzheimer’s and P. gingivalis may be well established, but it’s still overlooked, according to some experts.
A case in point is The Lancet’s international commission for dementia prevention, intervention, and care. The commission releases reports every few years about important insights into Alzheimer’s. Its last report came out in 2020, 6 months after the Science Advances-published study.
Functional dentist Dr. Mark Burhenne was disappointed that the report omitted any mention of the P. gingivalis connection.
“It was shocking to me that we’re not including gum disease as a risk factor. To me, it should be number one,” Dr. Burhenne told The Epoch Times. “We have a causal link now. If you can prevent gingipain from getting to the brain, then you’re in good shape.”
Given that gum disease is easily visible and has an established causative link to Alzheimer’s, some argue that dentists should be playing a more significant role in the battle against this degenerative brain disease.
The Commission’s Findings
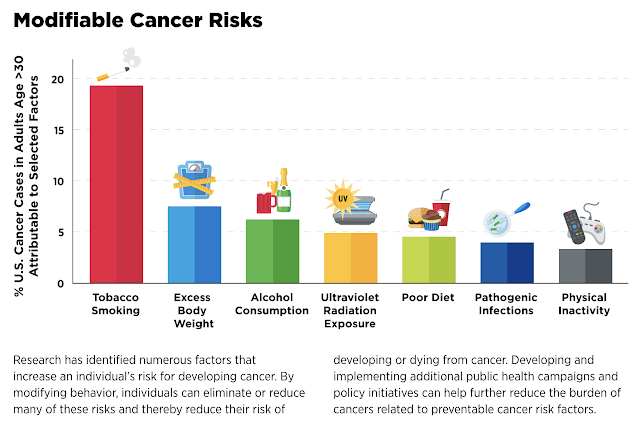
The Lancet commission published its initial findings in 2017 showing that less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact were factors associated with dementia risk. Three years later, it added excessive alcohol consumption, traumatic brain injury, and air pollution due to “newer, convincing evidence.”
The latest report was published in July 2020 in The Lancet, concluding that “together the 12 modifiable risk factors account for around 40 percent of worldwide dementias, which consequently could theoretically be prevented or delayed.”
Alzheimer’s disease is one of many forms of memory loss, but there are a variety of studies that find that many modifiable risk factors can help reverse these effects through lifestyle changes—if enacted in the early stages. New research indicates that Alzheimer’s can even be screened in preclinical stages through the gut microbiome.
The Epoch Times reached out to the head of the commission, Gill Livingston, to ask why gum disease was omitted from The Lancet’s list. She said dental health is a topic they are considering for the next update, which is expected in June 2024.
“It’s discussed in the next Lancet commission, and I therefore cannot say much,” Ms. Livingston, professor of psychiatry of older people at the University College in London, wrote via email. “But you might want to ask whether people with bad dental health are likely to be less or more educated, wealthier, and healthier.”
The Cost of Dental Care
There’s a major disconnect between the medical and dental professions when it comes to the holistic, systemic connections of health—and also in dental insurance coverage. Medicare coverage only extends to dental emergencies and doesn’t reimburse the costs of basic dental cleanings, fillings, and dentures.
Dr. Burhenne said that often, people won’t pay for any health expenses not covered by insurance, even if they’re able to budget for it. He relayed the story of one patient who had a great salary and benefits, but when he retired—even though he likely could have afforded the out-of-pocket expenses of cleanings and maintenance—he stopped coming. That patient developed gum disease and dementia rapidly.
Dr. Burhenne said that, ideally, patients ought to find a functional dentist who understands the systemic danger of gum disease on the entire body and recognizes it as a metabolic, autoimmune disease. However, insurance rarely covers expenses related to these professionals.
“I realize when I discuss all this, I’m telling everyone what to do, and it’s not as easy as it sounds. A lot of things have to change,” Dr. Burhenne said. “People are better when they have insurance. We need insurance for the retired.”
Medicaid, health care coverage for the poor, isn’t much better, although New York state is currently implementing expanded coverage, in part due to a lawsuit challenging the state’s stance that only four back teeth in addition to the front teeth are necessary.
Gum disease is the leading cause of tooth loss in adults. That’s why dental care is vital for screening and educating patients, even if dentists don’t acknowledge the connection between periodontitis and other diseases. Oral health habits—such as proper brushing and flossing—can prevent gum disease.
For anyone losing teeth or exhibiting other symptoms of gum disease well before they enter their golden years, intervention could go a long way toward preventing dementia, too.
Dr. Burhenne suspects that there will eventually be an affordable test for gingipain levels. Right now, the technology is too expensive and inaccessible. And while there may ultimately be a pill or mouthwash that targets gingipains, it could come with unwanted side effects or still be somewhat ineffective.
On the other hand, there are ways to prevent gum disease and preserve the good bacteria in the mouth that help maintain balance in the oral microbiome, which is the total collection of microorganisms, predominantly bacteria, that reside in the mouth.
Reversing Gum Disease Naturally
Boosting the good bacteria in a microbiome helps the environment achieve homeostasis. Katherine Dahl learned that lesson first with her gut, when she was able to use probiotics for a severe bacterial infection caused by Clostridioides difficile, better known as C. diff. But she still had cavities and poor oral health after three pregnancies.
“Dentists tend to be, ‘This is what I do: heal teeth, fill cavities, and make sure the mouth is functioning properly,’” Ms. Dahl said. But dentists don’t address the bacterial dimension to oral health, something she thinks could be a part of their responsibilities.
“We can disrupt the biofilm and then put new bacteria on the scene,” she said.
Biofilm in the mouth is bacteria that clump together and form plaque. New techniques can actually test saliva for the balance of bacteria, Ms. Dahl said, and allow people to detect signs of disease far before symptoms emerge. Her experience of using oral probiotics successfully prompted her to launch a new oral probiotic product with the help of her family of dentists.
Dr. Burhenne recommends probiotics to his patients and teaches dentists to incorporate oral microbiome testing. With his online and podcast presence, he educates the public on how to monitor their own gum health regularly.
“You can look at Google images of gum disease and look in the mirror, and you as a lay person could potentially have a good idea of where you’re at,” he said. “You don’t even need a test. You don’t need a dentist. Certainly, if you’re spitting in the sink after brushing and you see a little blood, that’s not healthy.”
Besides brushing your teeth after eating and flossing a few times a week, other lifestyle choices can help prevent gum disease, including:
- Avoiding mouthwash and other dental products that are disinfectants or antibacterial, as they kill off even the commensal, or good, bacteria.
- Eating a whole food diet and avoiding processed foods.
- Avoiding glyphosate, emulsifiers, and GMOs, which can damage the microbiome.
- Not drinking or eating from plastics, which are linked to systemic inflammation.
- Avoiding mouth breathing and dry mouth and boosting saliva production.
Some dentists may disagree, Dr. Burhenne said, but many of these practices actually contribute to gum disease by destroying the microbiome.
“It’s about having the right philosophy on what is the root cause of oral disease,” Dr. Burhenne said. “Unfortunately, most dentists aren’t there yet. They’re great clinicians, but they’ve been taught in the curriculum that you really need to disinfect the mouth.”
Reposted from: https://www.theepochtimes.com/health/an-important-and-overlooked-cause-of-alzheimers_5364392.html





.png)

Comments
Post a Comment